Oldest human record not broken for 28 years – are we making any progress with maximum lifespan?
Will Jeanne Calment’s record 122 years ever be broken?
Join the club for FREE to access the whole archive and other member benefits.
As our life journey unfolds, we transform from carefree youngsters, blissfully ignorant of our health, to enlightened individuals committed to safeguarding our well-being. When the golden years arrive, we often greet them with a newfound sense of urgency, fully aware of the trials ageing may bring. Eagerly, we embrace invigorating routines of regular exercise and nourishing diets, fueling our aspirations to retain youthful vigour and heighten our odds of a flourishing, extended lifespan.

Yet, with time, a thought-provoking question arises: why does the likelihood of illness and the realisation of our mortality intensify? This blog aims to unravel the omnipresent phenomenon of exponential growth in mortality and disease, delving into the underlying factors driving this trend.
The COVID-19 pandemic brutally reminded everyone of their vulnerability to mortality. However, special attention and precautions were always directed towards the elderly population, considering the significant impact of the virus on the population.
Extensive research has shed light on the profound influence of age on the severity and outcomes of COVID-19. The risks associated with COVID-19 escalate exponentially with age. As per reports, adults aged 65 and above accounted for 80% of hospitalizations and faced a striking 23-fold greater risk of mortality compared to individuals under 65[1]. For instance, in the UK, the likelihood of COVID-19-related deaths is less than 1 in 1,000 for age groups up to 60-69. However, this figure increases to 2, 7, and 18 in every 1,000 individuals for ages 70-79, 80-89, and 90 and above, respectively[2].
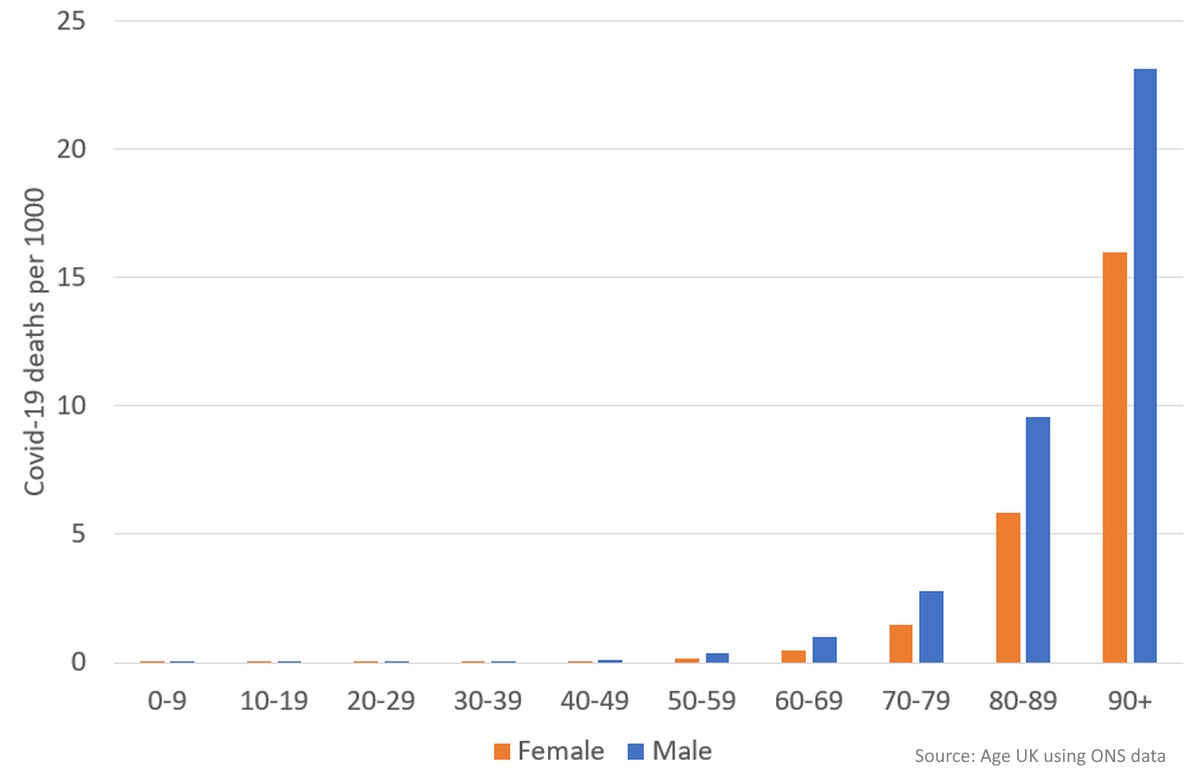
Even with critical care interventions, the risk of mortality exhibits an exponential increase with age. Roughly 40% of individuals undergoing critical care for coronavirus ultimately face mortality. However, the impact varies across age groups, with older individuals encountering higher vulnerability. Patients under 50 years old experience a 20% mortality rate, while those in their 50s face a rate of 40%. This rate escalates to 50% for individuals in their 60s and reaches approximately 60% for patients aged 70 and above[2].
The exponential rise in mortality and disease prevalence with age extends far beyond the realm of COVID-19, shedding light on a consistent pattern that resonates across various medical scenarios.
In fact, the mortality rates in the United Kingdom, spanning a period from 1984 to 2014 and projecting into the future until 2064, follow a distinct trajectory, starting with higher rates at birth, followed by a decline during adolescence, and then a subsequent exponential rise throughout adulthood and beyond[3].
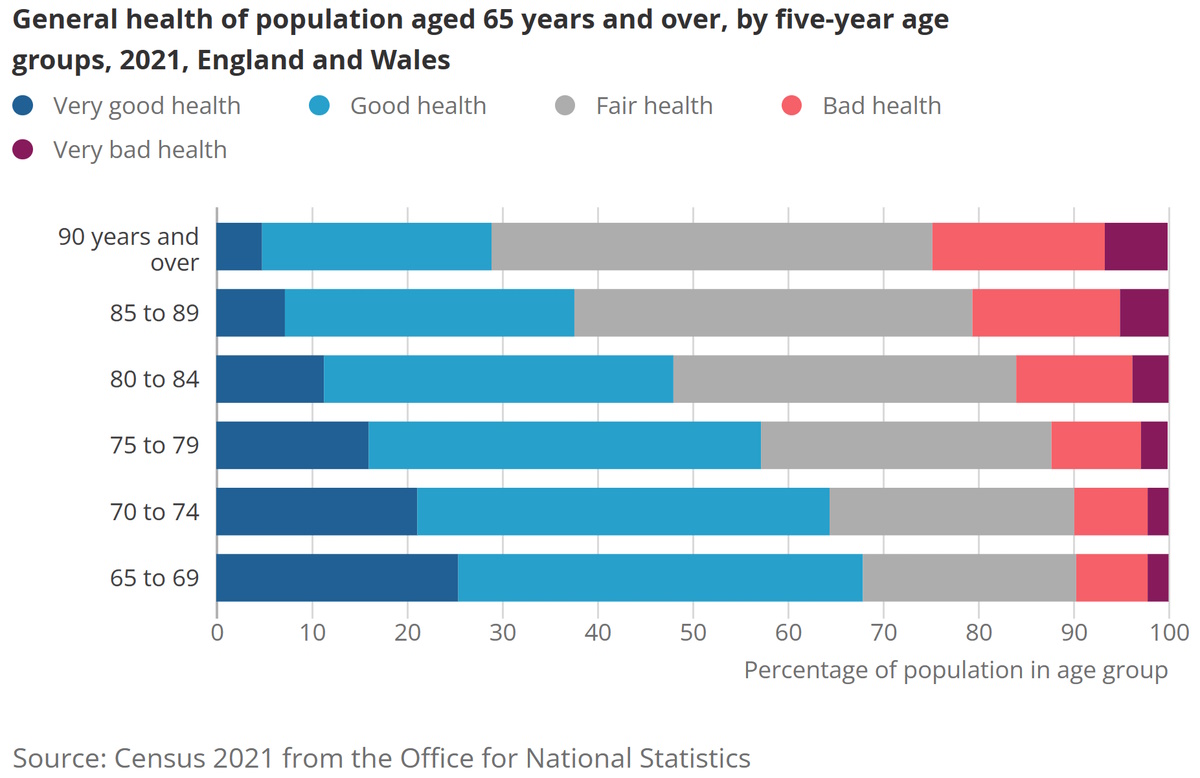
Fast forward to 2021, and an intriguing correlation between age and health status emerges among the older population in England and Wales. Notably, the prevalence of bad health exhibits a progressive increase across different age groups, beginning at 7.5% in the 65-69 age group and steadily climbing to a significant 18.1% among those aged 90 and above[4].
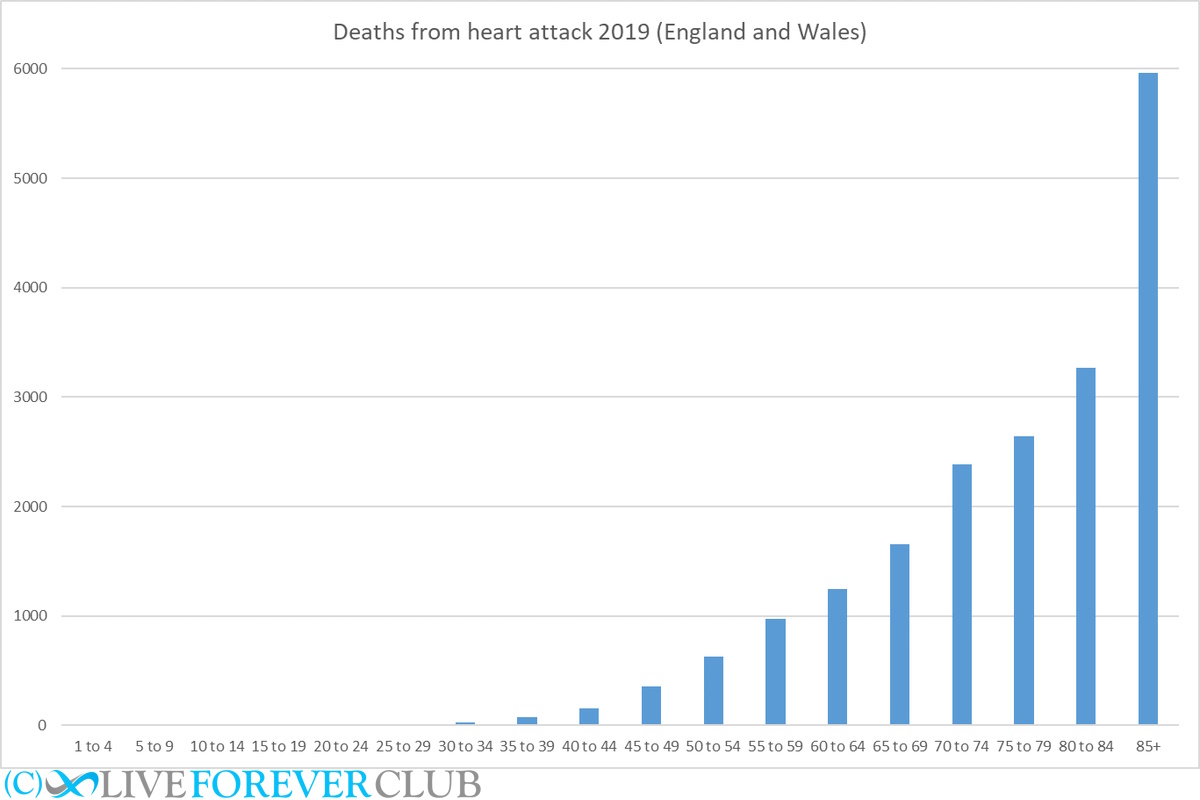
During the years 2019 to 2021, there is an observable upsurge in heart attack fatalities across various age groups in England and Wales, with a particular emphasis on the exponential surge among individuals as they advance in age. This consistent pattern of heightened mortality rates with ageing becomes especially pronounced among individuals aged 85 and above[5].
A clear association between age and cancer mortality is also evident. While children aged 0-14 and teenagers/young adults aged 15-24 account for a negligible fraction of cancer-related deaths in the UK, the majority of such deaths occur among adults aged 50-74 (42%) and those aged 75 and above (54%)[6].
Furthermore, a study involving 8,312 participants from England reveals a similar link between age and the prevalence of albuminuria, a crucial marker for chronic kidney disease. The risk of albuminuria reaches its lowest point in the 35-5 4 age group, at a mere 5.3%. However, it takes an exponential leap among individuals aged 55-64 (8.1%), 65-74 (11.7%), and 75 and above (17.9%)[7]
The data published in the Health Profile for England 2017 also underscores the observation that the morbidity rate among individuals in their late 80s was nearly twice as high as that of people in their early 60s. This finding encompasses a wide spectrum of diseases, such as cardiovascular disease, Alzheimer's and dementia (neurological disorders), and diabetes, all exhibiting a distinct pattern of exponential escalation as age advances[8].
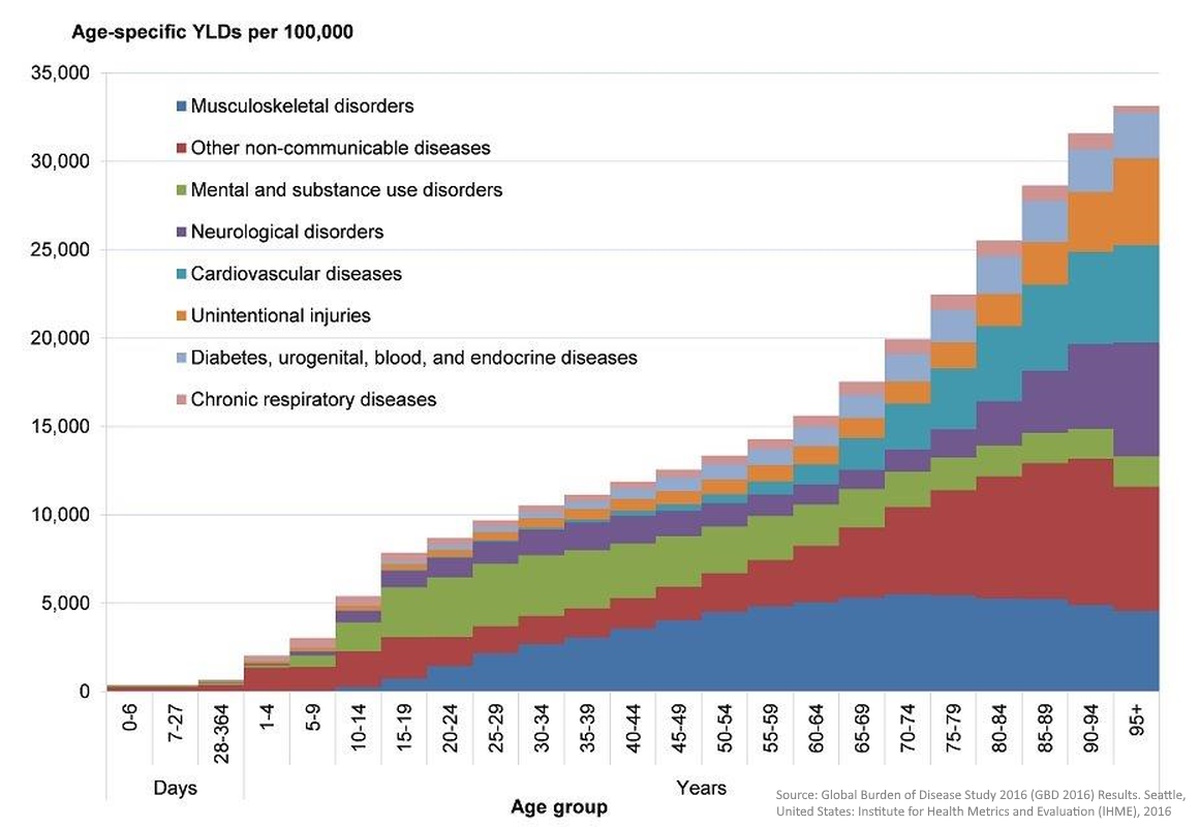
Overall, extensive research especially on non-communicable diseases consistently reveals the profound influence of ageing on health and related mortality.
Diseases and mortality follow a clear pattern of exponential increase as individuals age, prompting a closer examination of the factors that contribute to this trend. While addressing specific diseases is important, it does not fully address the ultimate cause of death, which is often attributed to old age itself.
Aside from COVID-19 and certain infectious diseases, most illnesses today are non-communicable and ageing plays a significant role in their development. The likelihood of developing non-communicable diseases rises substantially as individuals grow older, particularly after reaching the age of 65. This increased risk can be attributed to various biological mechanisms intricately linked to the ageing process.
As individuals age, their bodies undergo noticeable changes, including alterations in the immune system. These changes involve a decrease in T-cell variety and continuous activation of the innate immune system. Unfortunately, these changes hinder the body's ability to effectively combat viruses like SARS-CoV-2, leading to severe damage and organ failure.
Furthermore, numerous biological mechanisms contribute to the exponential surge in mortality and disease. These mechanisms encompass cellular senescence, telomere shortening, chronic inflammation, hormonal alterations, and mitochondrial dysfunction. Presently, researchers are directing their attention toward targeting these underlying mechanisms in order to unravel the enigmatic aspects of longevity and potentially extend lifespan.
In addition to biological factors, genetic predispositions, lifestyle choices, environmental influences, and socioeconomic factors can also contribute to the increased mortality rates associated with ageing. Unhealthy lifestyle choices, exposure to environmental toxins, and genetic factors can expedite the ageing process and elevate the risk of age-related diseases.
The exponential rise in mortality and diseases as individuals age is a remarkable phenomenon observed across various medical scenarios. Whether it's the devastating impact of COVID-19, the prevalence of chronic conditions, or age-related diseases, the data consistently highlights the profound effect of ageing on health outcomes.
Key biological mechanisms intricately linked to the ageing process, such as changes in the immune system, cellular senescence, chronic inflammation, and hormonal alterations, contribute significantly to this surge. Unravelling underlying mechanisms and focusing on them hold great promise for understanding longevity and potentially extending the human lifespan.
As we navigate the complexities of ageing, it becomes increasingly vital to prioritise healthy lifestyles, disease prevention, and innovative research. These efforts are crucial in mitigating the impact of this exponential increase and ensuring a healthier future for all.
1. A. L. Mueller, M. S. McNamara, and D. A. Sinclair, “Why does COVID-19 disproportionately affect older people?,” vol. 12, no. 10, pp. 9959–9981, May 2020, doi: https://doi.org/10.18632/aging.103344.
2. Age UK, Jun. 09, 2020.
3. J. Mills, “Past and projected data from the period and cohort life tables,” Ons.gov.uk, Dec. 11, 2015.
4. “Profile of the older population living in England and Wales in 2021 and changes since 2011,” Ons.gov.uk, Apr. 02, 2023.
5. “Heart attack deaths in 2019, 2020, 2021 and 2022 - Office for National Statistics,” Ons.gov.uk, 2019.
6. “Cancer mortality by age,” Cancer Research UK, May 13, 2015.
7. H. O. Hounkpatin et al., “Prevalence of chronic kidney disease in adults in England: comparison of nationally representative cross-sectional surveys from 2003 to 2016,” vol. 10, no. 8, pp. e038423–e038423, Aug. 2020, BMJ Open
8. Chapter 3: trends in morbidity and risk factors,” GOV.UK, Sep. 10, 2018.
Clock Foundation’s GrimAge Biological Age Test Review
Choosing supplements - why all supplements are not the same
Will Jeanne Calment’s record 122 years ever be broken?
Has this century seen extraordinarily long-lived Wimbledon champions, or are winners over 30 years of age the new normal?
Not as long as you might think. For radical life extension we need to reverse ageing.
What consumer tests are available to check your hallmarks of ageing and how they're impacting your body?
The biology of ageing looks at way more than just the genome and microbiome - here's 20 to start with!