Ageing is universal, yet it doesn’t happen the same way for everyone. One of the fascinating aspects of ageing is how it differs between men and women. On average, women live longer than men, but they also face unique age-related health issues. While women tend to experience frailty, men often encounter a higher incidence of severe age-related diseases like heart disease and certain cancers. Understanding why these differences exist can help us develop better, more personalized treatments for ageing-related conditions in both sexes.
Recent studies explore how sex differences affect the biological processes behind ageing. This growing field of research is known as “sex-based ageing biology.” By studying sex chromosomes, hormones, and cellular mechanisms, scientists are uncovering why men and women age differently at a molecular level. The implications of this research are significant, as it could lead to sex-specific approaches to prolonging health and longevity. Let’s dive into the biological foundations that set the stage for these differences.
Sex Chromosomes and Hormones:
The difference between male and female ageing starts with our chromosomes and hormones. Humans have two types of sex chromosomes: X and Y. Females typically have two X chromosomes (XX), while males have one X and one Y (XY). This difference affects everything from DNA repair to hormone production.
Sex Chromosomes and Lifespan
Females’ XX chromosome setup provides an advantage. In females, one X chromosome is mostly “switched off” through a process called X-inactivation, but some genes escape this inactivation, offering a “backup” that males don’t have. This extra gene protection may contribute to the longer average lifespan seen in women.
Sex Hormones and Healthspan
Sex hormones like estrogen and testosterone also play essential roles in ageing. Estrogen, the primary female sex hormone, protects against oxidative stress, which can damage cells. Testosterone, the main male hormone, influences metabolism and muscle health. As men and women age, hormone levels decline, with men experiencing gradual testosterone loss and women facing an abrupt drop in estrogen after menopause.
This hormonal shift makes women more vulnerable to bone density loss and other ageing-related issues after menopause, while men may see slower changes in muscle mass and metabolism.
Understanding these biological differences can help us better approach age-related diseases with treatments tailored to each sex.
The Hallmarks of Ageing
Ageing is driven by a set of cellular processes that scientists call the “hallmarks of ageing.” These include genomic instability, telomere shortening, loss of proteostasis, cellular senescence, and more. Let’s look at how these hallmarks vary between sexes and contribute to the different ways men and women experience ageing.
1. Genomic Instability: The DNA Repair Factor
Genomic instability refers to the accumulation of DNA damage over time, which can lead to mutations and age-related diseases like cancer. Men and women differ in how their bodies handle DNA repair. For example, some DNA repair mechanisms are less effective in women’s cells as they age, increasing their risk for certain cancers. The X chromosome contains several DNA repair genes, which may partly explain why women have a protective advantage over men, despite higher cancer rates in ageing men.
2. Telomere Attrition: Why Men’s Telomeres Shorten Faster
Telomeres are protective caps at the end of chromosomes that shorten as cells divide. Shortened telomeres signal cells to stop dividing, leading to ageing. Interestingly, men’s telomeres tend to shorten faster than women’s, partly due to the protective effect of estrogen, which boosts the enzyme telomerase. Telomerase helps lengthen telomeres, but as estrogen declines with age, women’s telomere length becomes more vulnerable.
3. Loss of Proteostasis: Protein Maintenance Differences
Proteostasis, or protein homeostasis, involves the creation, folding, and disposal of proteins within cells. When proteostasis fails, damaged proteins accumulate, leading to diseases like Alzheimer’s. Women’s cells generally manage protein maintenance better, thanks to their higher proteostasis activity, particularly in brain and muscle tissues. This may explain why women tend to develop neurodegenerative diseases later than men.
4. Cellular Senescence and Inflammaging: Differences in Immune Ageing
Cellular senescence refers to the state when cells stop dividing and accumulate, often leading to inflammation—a process known as inflammaging. Men tend to accumulate more senescent cells than women. This buildup contributes to a higher rate of inflammation in ageing men, which is linked to diseases like heart disease and type 2 diabetes. Women, on the other hand, have a more robust immune response, which helps clear senescent cells but also makes them more prone to autoimmune diseases.
5. Stem Cell Exhaustion: Gender-Specific Tissue Regeneration
As we age, our stem cells lose the ability to regenerate tissues effectively. This exhaustion occurs differently in men and women. Female mice, for example, show slower stem cell exhaustion than males, possibly due to estrogen’s protective effects. In humans, these differences suggest that men may experience faster declines in tissue regeneration, particularly in muscle and bone.
These cellular-level differences provide a roadmap for understanding why men and women face different health challenges as they age.
The Influence of Sex Hormones on Ageing
The effects of estrogen and testosterone extend beyond reproductive health; they also significantly influence ageing processes.
Estrogen’s Protective Role
Estrogen offers protection against oxidative stress, helping cells to repair damage efficiently. For example, in brain cells, estrogen reduces oxidative damage, potentially delaying cognitive decline in women. However, the decline in estrogen after menopause accelerates ageing in women, leading to issues like osteoporosis and cardiovascular disease.
Testosterone and Metabolic Health
Testosterone helps maintain muscle mass and supports metabolic health in men. Lower testosterone levels in older men contribute to muscle loss, which affects metabolism and increases the risk of obesity and diabetes. Studies suggest that testosterone therapy can help counteract some ageing effects, but its benefits and risks vary between individuals.
Hormone Therapy: A Double-Edged Sword?
Hormone therapy, particularly estrogen replacement, has been proposed as a way to combat ageing-related health issues in postmenopausal women. Research shows that hormone therapy can help maintain bone density and reduce the risk of osteoporosis in women. However, hormone therapy has associated risks, such as an increased risk of breast cancer and cardiovascular issues.
For men, testosterone replacement therapy has shown some promise in restoring muscle mass and metabolic function. However, it also comes with risks, including cardiovascular complications. As a result, researchers emphasize the need for personalized hormone therapy plans that consider individual health profiles and risk factors.
Emerging Research and Future Directions
Although we’ve made significant strides in understanding sex-based ageing, there’s much more to learn. Some key areas for future research include:
Role of the X Chromosome in Ageing
In females, one X chromosome is inactivated, but some genes still “escape” this process and contribute to cellular functions. Understanding how these genes influence ageing could reveal why women have resilience against certain age-related diseases.
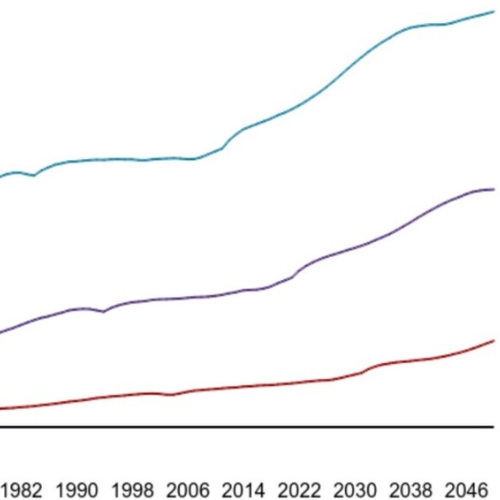
Sex-Specific Epigenetic Clocks
Epigenetic clocks track ageing by measuring DNA methylation patterns. Emerging studies suggest that men and women may age at different rates on an epigenetic level. Further research on these clocks could help refine age predictions and develop sex-specific anti-ageing interventions.
Personalized Medicine for Ageing
With a better understanding of sex differences in ageing, we can create more personalized treatments. For example, adjusting drug dosages and treatments based on sex could lead to more effective interventions for age-related diseases in both men and women.
Inclusion of Sex as a Variable in Clinical Studies
Historically, many clinical trials excluded women, resulting in a lack of data on how treatments work in female patients. The National Institutes of Health (NIH) now mandates the inclusion of both sexes in research studies. This shift will help us understand how treatments affect men and women differently and allow for more accurate data on age-related diseases.
Conclusion
The journey of ageing affects men and women differently. From the molecular level of chromosomes and hormones to the visible impacts on healthspan and lifespan, sex plays a crucial role in how we age. The insights we gain from studying these differences can revolutionize ageing research and lead to more effective treatments for age-related diseases in both sexes.
For individuals and healthcare providers, understanding these sex-based differences highlights the importance of a personalized approach to ageing. With advancements in research, we can hope for a future where both men and women can age healthily and enjoy longer, more fulfilling lives.
The study is published in the journal Open Biology. It was led by Maria Felicia Basilicata from the Institute of Molecular Biology (IMB), Mainz, Germany.