As populations age across the globe, the challenge of maintaining strength and independence in later years becomes urgent. Millions of older adults struggle with conditions like sarcopenia and frailty, which strip away mobility and self-sufficiency. Researchers have explored many treatments—from exercise programs to hormone therapies—but drug options remain limited. Among the most studied possibilities stands metformin, a drug long known for managing type 2 diabetes.
Scientists hoped that metformin’s broader impact on ageing-related biology could make it useful beyond blood sugar control. Could this familiar medication become a tool for preserving physical performance in older people with declining strength? A major UK trial set out to answer this question. The results offer a clear response—and a cautionary tale about trying to repurpose drugs without strong evidence.
The Burden of Sarcopenia and Frailty in Later Life
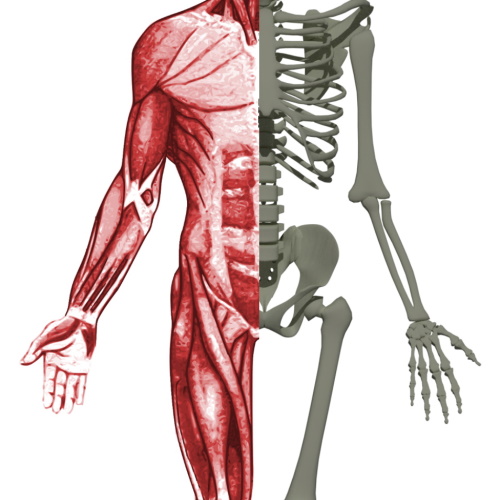
Sarcopenia, the gradual loss of muscle mass and strength with age, reduces mobility and increases risk of falls, dependency, and premature death. It forms the core of physical frailty—a syndrome marked by fatigue, weight loss, weakness, slow walking speed, and low physical activity. This combination often leads to longer hospital stays, reduced quality of life, and increased reliance on care services.
Resistance training remains the best-known strategy to counteract these effects. But it’s not feasible for everyone. Many frail individuals cannot follow structured exercise routines due to pain, comorbidities, or disability. So there is growing interest in medications that might improve muscle function and help slow physical decline. Metformin, thanks to its broad effects on ageing biology, emerged as one of the top candidates.
Why Metformin Was Chosen for This Trial
Beyond its use in diabetes, metformin has shown potential in affecting pathways tied to ageing. It interacts with mTOR signalling, mitochondrial function, chronic inflammation, and even the gut microbiome. It may reduce cellular stress and modulate immune responses. Some studies have hinted that it might reduce the risk of frailty and muscle loss in people with diabetes.
One earlier trial showed that older people with prefrailty who took 500 mg of metformin three times daily for 16 weeks improved their walking speed. Another trial in older men with sarcopenia noted a small boost in grip strength. But these findings came from small groups and lacked consistency. The MET-PREVENT trial aimed to test this drug more rigorously, in a group of older people with probable sarcopenia and physical prefrailty or frailty.
A Rigorous Study Design to Address an Important Question
Conducted in Gateshead and Newcastle, England, the MET-PREVENT trial followed a gold-standard design. Researchers recruited 72 participants aged 65 and older, all with slow walking speeds and signs of muscle weakness. Half received 500 mg of metformin three times daily for four months. The other half took a placebo. Neither the participants nor the researchers knew which group each person was in.
The primary measure of success was improvement in walking speed over four metres—a simple but powerful predictor of health outcomes in older adults. Secondary outcomes included grip strength, muscle mass, quality of life, and ability to perform daily tasks. The researchers also closely tracked any side effects or adverse events.
Clear Result: No Benefit Found from Metformin
At the end of four months, the results were disappointing. Walk speed did not improve in the metformin group compared to placebo. Grip strength and other measures of physical performance also showed no significant differences. Muscle mass remained the same. There was no gain in quality of life or ability to carry out daily activities.
“Metformin did not improve 4-m walk speed and was poorly tolerated in this population,” the authors noted.
This finding held true even after accounting for sex, baseline strength, and adherence. Participants who took their medication exactly as prescribed saw no advantage over those in the placebo group. The research team tested for possible subgroup differences, such as sex or insulin resistance, but none of these changed the outcome.
Side Effects Raise Further Concerns
More than lack of benefit, the trial revealed something more troubling: metformin was poorly tolerated. Every participant in the metformin group reported at least one adverse event. One-third required hospitalisation during the study. Common side effects included diarrhoea, nausea, vomiting, and elevated plasma lactate levels. Many participants stopped taking the medication due to discomfort.
The discontinuation rate in the metformin group was almost triple that of the placebo group. Even among those who completed the trial, nearly half had suboptimal adherence. These findings raise important concerns about prescribing metformin to frail older people, especially at doses used in this trial.
Why Didn’t Metformin Work? Possible Explanations
The researchers explored several explanations. One theory suggests the high dropout rate diluted any real benefit. But the data from those who adhered closely to the regimen still showed no improvement. Another possibility is that the dose was either too low to be effective or too high to be well tolerated.
Interestingly, other studies in healthier older people found that metformin could blunt the benefits of exercise, possibly by interfering with muscle-building pathways. This raises the idea that metformin may suppress some of the very mechanisms needed to improve strength and performance.
As the authors note, “The number and complexity of metformin’s actions on biological pathways relevant to muscle health challenges our ability to understand why metformin did not improve physical performance in the current trial.”
Limitations and Strengths of the Study
One major strength of the MET-PREVENT trial lies in its ability to recruit and retain a vulnerable group often excluded from research. The trial design was robust, with careful control and masking. Walk speed, chosen as the main outcome, is strongly linked to survival, independence, and risk of falls. Yet the study also faced challenges.
The sample was small, limiting the ability to detect modest effects. The trial only ran for four months. Some benefits from metformin might take longer to appear. The population was not diverse, with nearly all participants being White British. Also, people with diabetes, kidney disease, or cognitive impairment were excluded, which limits how widely these findings apply.
What This Means for Future Research and Practice
The trial's results suggest metformin is not a good candidate for improving physical function in older adults with significant frailty or sarcopenia. However, future studies could explore its use in less impaired populations. Two earlier trials that showed benefits focused on older adults with prefrailty, who had better walk speed at the start.
“Our results suggest that metformin is unlikely to be a suitable geroprotective agent for long-term use by older people with sarcopenia and frailty or prefrailty,” the authors note.
This study also highlights the importance of matching the right intervention to the right group. A treatment that works for healthier older adults may not help—or may even harm—those who are more frail. Researchers must continue to explore treatments that are both effective and safe for this population.
Conclusion: Not the Solution We Hoped For
In the quest to improve healthspan in ageing populations, metformin has received much attention. But the MET-PREVENT trial offers a sobering reality check. In frail older adults with low mobility, metformin did not deliver. Its use brought more side effects than benefit.
The need for effective interventions in sarcopenia remains high. But this trial reminds us that even promising drugs must pass the test of real-world impact. Exercise, though challenging for some, remains the best strategy for now. The search for other treatments continues—but metformin, it seems, is not the answer for this group.
The study is published in the journal The Lancet Healthy Longevity. It was led by Prof Miles D Witham, PhD from Newcastle University.