Ageing remains one of the greatest biological puzzles. As the years pass, our bodies lose their fine-tuned harmony. Wrinkles may mark the surface, but deep within, vital organs like the heart grow tired. The heartbeat slows, muscle fibers stiffen, and energy production begins to fade. What if part of this shift isn’t purely genetic or inevitable? What if the gut, long known for its role in digestion, influences how the heart ages?
A new study by researchers at Shanxi Medical University dives deep into this idea. Their work explores whether the gut microbiota—the trillions of bacteria living in our intestines—affect natural heart ageing. Using an innovative rat model, they reveal a surprising link between gut bacteria, metabolism, and cardiac health.
Why the Gut May Matter More Than We Thought
The gut microbiota affects many systems beyond digestion. It communicates with the immune system, shapes inflammation, and even influences hormones. During ageing, gut composition changes. Diversity drops. Harmful bacteria often rise. These shifts are not just passive. They can trigger immune responses, weaken the intestinal barrier, and leak toxic substances like lipopolysaccharides into the bloodstream.
That can set off inflammation across the body—including in the heart. Chronic inflammation plays a central role in ageing and cardiovascular disease. But until now, most studies focused on how gut bacteria worsen heart disease. Few have asked how they affect normal, healthy heart ageing. This study addresses that gap.
An Experiment That Crosses Generations
To test their hypothesis, scientists performed fecal microbiota transplantation (FMT) between rats of different ages. They transplanted gut bacteria from young rats into old ones, and vice versa. Then they watched closely for signs of change.
The heart was their main focus. They used echocardiography to examine structure. PET-CT imaging tracked diastolic function. Advanced tools measured ATP levels, mitochondrial shape, and energy metabolites. Western blotting showed how key proteins in glucose and fat metabolism behaved after FMT. The goal was to understand how age-related gut microbiota could reshape heart metabolism.
Old Hearts Show Structural Decline
Before any transplant, the researchers examined the hearts of young and aged rats. Old rats had thicker left ventricular walls and stiffer interventricular septa. Yet their systolic function, or ability to contract and pump blood, remained normal. It was the relaxation phase—diastole—that suffered.
PET-CT scans confirmed this. Aged rats had slower early diastolic filling. Their hearts couldn’t relax and fill with blood as efficiently. Microscopic analysis revealed disorganized heart muscle cells, enlarged intercellular spaces, and visible hypertrophy. These are classic signs of age-related cardiac remodeling.
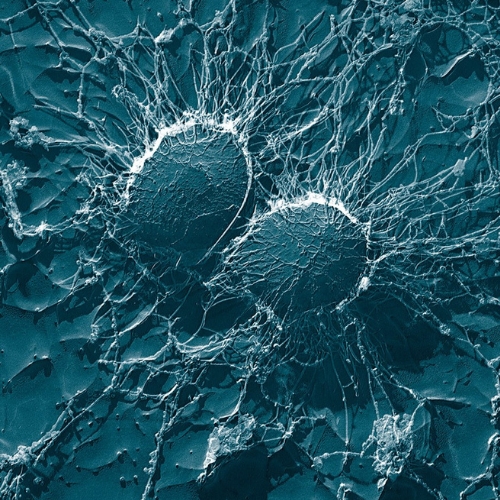
Ageing Also Hits the Mitochondria
Mitochondria fuel the heart. They generate ATP, the energy needed for every beat. In older rats, ATP levels dropped. The mitochondria looked swollen, irregular, and full of vacuoles. Their cristae—the internal folds critical for energy production—were often disrupted. Fewer glycogen granules surrounded these energy centers, hinting at weaker fuel reserves.
At the molecular level, protein levels for CPT1A and GLUT-4 dropped. These proteins help metabolize fatty acids and glucose, the heart’s main fuels. The findings pointed to one conclusion: ageing guts come with ageing hearts, and energy production takes a hit.
FMT from the Young Brings Fresh Energy
Then came the transplant. Old rats received gut bacteria from young donors. Within weeks, their hearts began to shift. Echocardiography showed thinner walls and more normal septal thickness. PET-CT revealed improved diastolic filling. Muscle fibers arranged themselves more neatly. Signs of hypertrophy declined.
At the mitochondrial level, structures looked healthier. There were more glycogen granules, less crista damage, and reduced vacuoles. ATP content rose. CPT1A and GLUT-4 expression also increased, suggesting a rebound in both fat and glucose metabolism.
Young rats who received old gut microbes faced the opposite. Their heart walls thickened. Diastolic function declined. Mitochondria swelled, and ATP production fell. These rats began to show early signs of cardiac ageing.
Gut Composition Shifts with the Transplant
The transplant didn't just affect the heart. It reshaped the microbiome itself. Aged rats who received young gut bacteria had increased diversity and richness. Certain bacterial groups known for promoting inflammation, like Flavonifractor and Oscillibacter, decreased.
Meanwhile, bacteria like Prevotella and Faecalibacterium rose. These microbes may help calm inflammation or enhance energy metabolism. The changes in gut composition closely mirrored the donor rats. This suggested that FMT effectively transplanted not just bacteria, but also some age-related traits.
Metabolites Tell a Parallel Story
LC–MS metabolomics offered another lens. After FMT, the metabolic profiles of recipient hearts moved toward the donor’s. Old rats gained metabolites tied to fatty acid oxidation and the TCA cycle—like malic acid and long-chain acylcarnitines. Young rats lost them when they received aged microbiota.
One metabolite stood out: linoelaidyl carnitine. It decreased with age and increased after FMT from young donors. This molecule helps transport fats into mitochondria. Its abundance correlated with the presence of Sutterella, a genus that rose in healthy ageing.
The shift in metabolites echoed the changes in heart energy. When the gut changed, the heart’s fuel system changed too.
Stress and Autophagy: The Silent Drivers
The study also measured oxidative stress and autophagy, two processes deeply involved in ageing. Old rats had more MDA, a marker of oxidative damage, and less SOD, an antioxidant enzyme. They also had a lower LC3II/LC3I ratio, indicating weaker autophagy.
FMT reversed these trends. Aged rats who received young microbiota produced less MDA and more SOD. Autophagy improved. The reverse transplant in young rats worsened these markers. Interestingly, the researchers found that spermidine, a known promoter of autophagy, followed the same pattern. This supports the theory that gut microbes may regulate ageing through autophagy.
Final Insights and Future Possibilities
This study does not promise eternal youth. But it opens a new window into how we age. The gut microbiota appears to influence heart health in complex, measurable ways. It changes structure, boosts or reduces energy, alters metabolites, and controls stress responses.
In rats, simply changing gut bacteria shifted the ageing trajectory of the heart. Old hearts regained youth. Young hearts took on signs of age. These transformations were not superficial. They touched every level of the heart, from whole-organ function to microscopic mitochondrial health.
The study raises important questions. Could this approach work in humans? Could diet, probiotics, or targeted bacterial therapies one day slow cardiac ageing?
For now, one thing is clear. The gut and heart are not strangers. They speak through molecules, microbes, and metabolic pathways. And in that quiet conversation may lie clues to a longer, healthier life.
The study is published in the journal Experimental Gerontology. It was led by researchers from Shanxi Medical University, Taiyuan, China.