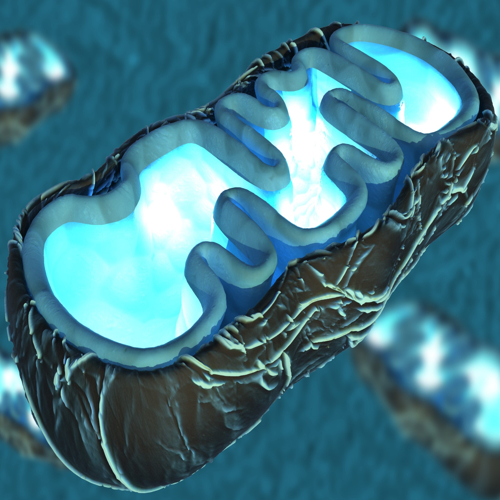
Mitochondria are tiny structures in our cells that keep us alive. They produce energy and help maintain cell health. When they stop working properly, cells lose power and start to fail. This dysfunction is linked to many diseases and to ageing. Mitochondria transfer and transplantation (MTT) bring fresh hope. By moving healthy mitochondria into damaged cells, scientists want to restore lost functions and improve health. This idea may sound simple, but it involves many complex steps and faces big challenges.
The vital role of mitochondria
Mitochondria are often called the powerhouses of the cell. They make ATP, the molecule cells use as fuel. But mitochondria do much more. They control cell death, help in making hormones, and balance calcium. When they fail, cells become weak. This leads to problems like neurodegenerative diseases, heart conditions, and muscle disorders. Researchers found that adding healthy mitochondria to sick cells improves energy levels and helps cells recover.
Studies show that MTT can boost ATP production and reduce harmful molecules. It also helps cells survive under stress. In animal studies, MTT improved tissue repair and reduced disease damage. This suggests that MTT could work for both sudden injuries and chronic diseases. However, the journey from lab to clinic is long and full of hurdles.
Natural ways cells share mitochondria
Cells have a natural way of sharing mitochondria. They use small tubes called tunneling nanotubes. These act like bridges between two cells. Through these bridges, mitochondria and other materials pass from one cell to another. Other methods include small vesicles and gap junctions. These natural ways are useful but not precise enough for therapy.
Researchers want to copy these natural systems to create therapies. But natural transfers cannot control where the mitochondria go. They also lack the precision needed to treat specific tissues. Because of these limits, scientists are working on engineered systems to improve accuracy and safety.
Current methods of delivering mitochondria
Several ways exist to deliver mitochondria to damaged tissues. One method is direct injection into organs like the heart or brain. This helps limit where the mitochondria go but requires surgery. Another way is to inject mitochondria into the bloodstream. This spreads them through the body but risks strong immune reactions and poor targeting. Intranasal delivery offers a non-invasive way to target the brain. However, it needs better efficiency and accuracy. Oral delivery is also being explored but faces big problems in the digestive tract.
All these methods share similar problems. Mitochondria can get damaged during isolation or delivery. They often face harsh conditions in the body, like high calcium levels or harmful molecules. Many mitochondria do not survive the journey or fail to enter the target cells. Making sure they stay alive and function well during delivery is a major challenge.
Improving delivery with biotechnology
New technology is helping scientists protect mitochondria and improve their uptake. Coating mitochondria with special molecules helps them pass into cells more easily. Cell-penetrating peptides are one option. These short, charged peptides help mitochondria cross cell membranes. Polymers and lipids are also used to shield mitochondria from immune attacks and physical stress.
Hydrogels act as soft carriers. They hold mitochondria and release them slowly at the target site. This improves survival rates and helps mitochondria blend into host cells. Engineered vesicles like liposomes and extracellular vesicles are also useful. These act as protective packages, delivering mitochondria safely to the right cells.
Engineered vesicles: tiny protectors
Extracellular vesicles (EVs) are natural carriers made by cells. They carry proteins, RNA, and sometimes even whole mitochondria. When used in MTT, EVs protect mitochondria from damage and keep them working longer. They can cross barriers like the blood-brain barrier. This makes them helpful for brain-related diseases.
Liposomes are artificial vesicles made from lipids. Scientists can modify them to target specific tissues or cell types. They help avoid immune responses and improve precision. Special molecules can be added to guide them exactly where they need to go. Once inside the target cell, these vesicles release mitochondria so they can start working.
Hydrogels: supporting local delivery
Hydrogels are soft, jelly-like materials that can hold mitochondria. When injected into damaged tissue, they slowly release mitochondria in that area. This local delivery keeps mitochondria near the target site, boosting their chance to help. Hydrogels also protect mitochondria from harsh conditions during transfer. They support better cell integration and improve tissue healing.
Materials like Pluronic F127 and hyaluronic acid are used to make these hydrogels. They do not harm mitochondria and allow for slow, controlled release. Studies show improved heart function, smaller damaged areas, and better cell survival when using hydrogel-based delivery.
Safety and immune system challenges
Even though mitochondria come from the body, they can still cause immune responses when transferred. Some studies report no reaction, but others show strong inflammation and cell damage. Protective coatings and surface changes help reduce these risks. Scientists continue to look for ways to avoid unwanted immune attacks.
Safety remains a major focus. It is critical to make sure mitochondria do not enter the wrong tissues or cause harmful effects. There is also a concern about genetic risks if mitochondria integrate into reproductive cells. Long-term effects are still not fully understood. More studies are needed to examine what happens over time.
Scaling production and regulatory issues
Taking MTT from lab experiments to actual patient treatments is not easy. Producing enough mitochondria requires tight control and advanced equipment. Each batch must be the same and meet strict safety standards. The process is expensive and complex. These factors make treatments costly and hard to access for many people.
Health authorities need strong evidence of safety and effectiveness. Regulations require detailed data before approval. Because mitochondria-based therapies are new, there are many unknowns. Clear rules and guidance are needed to help bring these treatments to patients.
Challenges with nanoparticles
Nanoparticles can help deliver mitochondria and improve targeting. But they can also harm cells and cause unwanted side effects. Managing these risks is essential. Nanoparticles need to be safe, stable, and able to avoid quick removal by the immune system. They must also reach target tissues in high enough amounts.
Delivering mitochondria to organs like the brain is especially hard. The brain has strong protective barriers that block many treatments. Better targeting and a deeper understanding of how nanoparticles work in the body are needed to improve success.
Ethical concerns and future directions
The source of mitochondria raises ethical issues. Using a patient’s own mitochondria lowers risk but is not always possible. Using donor mitochondria can introduce unknown genetic risks. There is a concern that donor mitochondria might pass on unwanted traits if they enter reproductive cells. There is also a risk of contamination during preparation, which can harm patients.
Cost is another barrier. Making and delivering mitochondria treatments is expensive. A cost analysis is needed to see if these treatments can become widely available. Scientists also want to know if mitochondria from different tissues work better for certain diseases. Engineered or artificial mitochondria could offer new options in the future.
Combining mitochondria with protective molecules may improve treatment results. This combined approach could protect cells better and make mitochondria more effective.
A new chapter in medicine
Mitochondria transfer and transplantation open a new way to treat diseases linked to mitochondrial failure. It offers hope for patients with few other options. But many challenges remain before it can become a standard treatment.
Researchers must focus on long-term safety and better delivery systems. Stronger safety checks and more studies are needed to understand the real impact of MTT. Once these challenges are solved, MTT could change how we repair tissues and fight diseases
The journey is long and will require teamwork across many fields. But the potential benefits are huge. One day, mitochondria therapies might help slow ageing, heal damaged tissues, and bring new life to failing organs. As science advances, MTT could become a key part of future medicine.
The study is published in the journal Nature Communications. It was led by researchers from Baskent University.