Obesity and type 2 diabetes mellitus (T2DM) are global health crises. These disorders drive heart disease, liver failure, nerve damage, and kidney dysfunction. Behind these complications lies a deeper problem—cellular senescence.
New science now suggests that removing these dysfunctional “zombie” cells could reverse metabolic damage and restore health.
What Is Cellular Senescence?
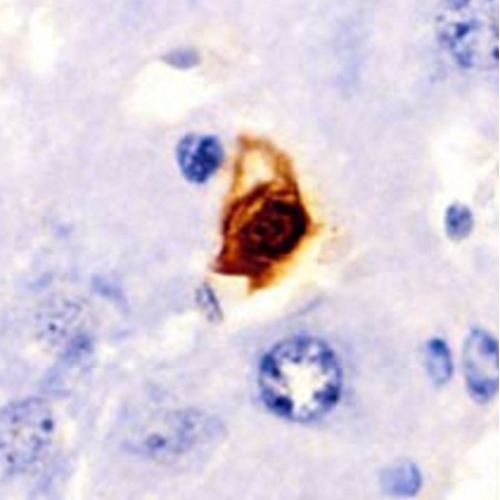
Senescent cells are stressed or damaged cells that stop dividing but remain alive. They produce harmful molecules—cytokines, enzymes, and growth factors—called the senescence-associated secretory phenotype (SASP).
SASP causes inflammation and spreads dysfunction to neighbouring cells. Senescent cells help in wound healing and cancer prevention briefly. But long-term, they cause chronic diseases and tissue damage.
Senescence in Obesity and Diabetes
Obesity and T2DM accelerate senescence. In obese people, fat tissue becomes a senescent hotspot. These cells release SASP, increasing inflammation and worsening insulin resistance.
In T2DM, high glucose levels push cells into early senescence across many organs—pancreas, liver, kidneys, and blood vessels. This deepens damage and drives disease progression.
The study shows how senescent cells affect major organs—damaging beta cells, fat tissue, retina, liver, and kidneys—leading to systemic metabolic failure.
Fat Tissue: Ground Zero for Senescence
Adipose tissue stores fat and also acts as an endocrine and immune organ. In obesity, it inflames and accumulates senescent cells. Visceral fat (around organs) holds more senescent cells than subcutaneous fat (under the skin).
Senescent fat cells release MCP-1, attracting macrophages that worsen inflammation. This impairs fat cell renewal, increases free fatty acids, and promotes T2DM.
Senescence in brown fat also causes “whitening,” where heat-producing brown fat loses function. Thermogenesis drops. Energy burns slower. Weight gain follows.
Pancreatic Beta Cells Fail with Ageing
Beta cells secrete insulin to regulate blood sugar. Senescence reduces their number, impairs mitochondrial function, and disrupts insulin release.
Ageing beta cells show less GLUT2, lower PDX1, and mitochondrial stress. They secrete more SASP, worsening local inflammation in the pancreas. This leads to beta-cell burnout and glucose imbalance.
Liver Steatosis and Senescence
Fatty liver disease, or MASLD, affects nearly 80% of people with diabetes. Chronic glucose stress causes hepatocytes to become senescent. They absorb more fat and lose export capacity.
Senescent liver cells also release IL-6, MCP-1, and TNF-α. These signals attract immune cells that trigger fibrosis. Hepatic stellate cells join in and build scar tissue. The disease progresses from steatosis to full MASH.
The study shows how senescence in the liver disturbs metabolism, drives inflammation, and blocks regeneration.
Kidneys Under Attack
Diabetic kidney disease (DKD) affects 40% of T2DM patients. Senescent cells build up in glomeruli and tubules. They trigger fibrosis through oxidative stress and SASP release.
AGEs (advanced glycation end-products) form during hyperglycaemia and drive kidney ageing. They activate pathways like NF-κB and TGF-β, promoting renal scarring and functional decline.
In kidney transplants, graft survival depends partly on the senescence level in donor tissue. High p16INK4a levels predict poor function post-transplant.
Senescence Fuels Heart Damage
Obesity and T2DM raise cardiovascular disease risk. High glucose and fatty acids damage vessels, promote senescence, and induce inflammation.
Senescent cardiac cells release growth factors like IGF1 and EGF that trigger fibrosis. Collagen buildup reduces heart flexibility and causes cardiomyopathy.
In mice, clearing senescent cardiac progenitor cells improved heart function and promoted regeneration.
Nervous System Degeneration
Diabetic neuropathy affects millions. Senescent glial and Schwann cells disturb nerve repair. SASP molecules like IL-6 and TNF-α slow signal transmission and impair healing.
Foot ulcers and infections follow, often leading to amputations. Transplanting MSCs can help, but diabetic patients have senescent stem cells with poor regenerative ability.
Retinal Senescence and Vision Loss
Diabetic retinopathy (DR) starts with microvascular damage. High glucose causes endothelial cell senescence in the retina. This impairs blood flow and triggers abnormal angiogenesis.
VEGF, IL-6, ICAM-1, and MMPs leak from senescent cells, damaging vision. SASP promotes vessel rupture, leading to vision impairment or blindness.
Lung Fibrosis in Diabetes
Diabetes-linked lung fibrosis often goes unnoticed. Senescent pulmonary lipofibroblasts produce fibronectin and collagen, stiffening the lungs.
TNF-α and TGF-β fuel this process. ROS damage alveolar cells. PAI-1 builds up fibrin. The lungs lose elasticity and scar over time, reducing breathing capacity.
Senolytics: Drugs That Kill Senescent Cells
Senolytics are compounds that selectively remove senescent cells. This prevents SASP-driven damage and inflammation.
Dasatinib + Quercetin (D+Q) is the best-known combination. Together, they destroy senescent cells and improve metabolic function. Clinical trials show benefits in fibrosis, kidney disease, and pulmonary function.
Fisetin, a natural flavonoid, reduces senescent burden in aged mice. It improves kidney and heart function and may extend lifespan.
Metformin improves insulin sensitivity and inhibits complex I in mitochondria. This activates AMPK and SIRT1, which help prevent senescence. Trials like TAME and MILES explore its effects on human ageing.
Other Senolytic Candidates
Rapamycin: Blocks mTOR, triggering death in senescent cells.
Resveratrol: Activates AMPK/SIRT1, promotes antioxidant defence.
NMN/NR: Restore NAD+ levels, support DNA repair and metabolism.
MitoTam: Mitochondria-targeted tamoxifen that kills senescent cells via ferroptosis.
Each drug targets different aspects of cellular ageing. Most are still under trial, but results look promising.
New Roles for Existing Diabetes Drugs
GLP-1 agonists like liraglutide may reduce senescence indirectly.
Tirzepatide, a dual agonist, reduces inflammation in fat tissue.
SGLT2 inhibitors lower oxidative stress and reduce senescent cell buildup in kidney, liver, and fat.
These drugs, already approved for diabetes, may soon help manage ageing-related decline.
Exercise: The Original Senolytic
Exercise clears senescent cells in fat, reduces inflammation, and improves insulin sensitivity. It boosts DNA repair, antioxidant enzymes, and immune clearance of damaged cells.
Active lifestyles protect organs and reduce metabolic stress, slowing the onset of obesity-related diseases.
Bariatric Surgery and Senescence
Surgery offers rapid improvements. Weight loss reduces senescent burden in fat and other tissues. Inflammation drops. Insulin sensitivity improves.
Markers of premature ageing decline post-surgery. Still, surgery isn’t suitable for all. Pharmacological senolytics remain vital for many.
Final Thoughts: The Future of Metabolic Therapy
Obesity and T2DM are rising fast. Current treatments manage symptoms but don’t stop disease progression. Senescence offers a new target—deep inside the biological engine.
Targeting senescent cells could reset tissue function, reduce inflammation, and reverse chronic complications. Drugs like D+Q, fisetin, and metformin might become first-line therapies.
Combining lifestyle, pharmacology, and cellular repair may lead to longer, healthier lives. We may soon treat metabolic disease by restoring cellular youth.
The future of obesity and diabetes care may not lie in just controlling blood sugar—but in targeting the age of our cells.
The study is published in the journal Frontiers in Cell and Developmental Biology. It was led by researchers from Charles University.