Meniscus injuries, common in athletes and active individuals, often lead to long-term joint issues and may contribute to osteoarthritis if left untreated. The meniscus is a crescent-shaped cartilage in the knee that helps cushion and stabilise the joint.
Damage to this structure, especially in the inner, avascular zone, can be problematic since it has a limited capacity for self-healing. For years, researchers have searched for effective solutions to restore the meniscus, but conventional approaches face challenges due to the tissue's unique properties.
One recent area of exploration involves cellular senescence—a biological state where cells stop dividing but remain metabolically active. Traditionally linked to ageing and degenerative diseases, cellular senescence has received a fresh perspective as scientists investigate its potential role in tissue repair.
A recent study on rats explored how senescent cells could influence spontaneous repair in the meniscus, suggesting that cellular senescence might offer a regenerative avenue in medicine. Below, we’ll dive into the fascinating findings and explore what they could mean for future therapies.
Understanding Cellular Senescence and SASP
Cellular Senescence: Friend or Foe?
Cellular senescence occurs when cells enter a permanent state of growth arrest, no longer dividing but remaining metabolically active. This phenomenon is generally triggered by factors like DNA damage, oxidative stress, or exposure to harmful chemicals.
These non-dividing cells release a mix of molecules called the Senescence-Associated Secretory Phenotype (SASP). SASP molecules include inflammatory cytokines, growth factors, and proteases, which impact the surrounding tissue.
Senescent cells have long been associated with ageing and disease because their inflammatory SASP factors can damage healthy tissues when they accumulate in large numbers.
However, recent research indicates that these same SASP factors can benefit tissues by stimulating repair mechanisms when present temporarily and in moderation. In certain contexts, senescent cells can promote wound healing and regeneration, helping repair structures like cartilage, skin, and even heart tissue.
SASP: A Key Player in Tissue Repair
The SASP produced by senescent cells is a complex mixture of bioactive molecules that interacts with neighboring cells. In tissue repair, SASP acts as a signaling tool, recruiting immune cells, stimulating cell proliferation, and encouraging extracellular matrix remodeling.
This dual nature of SASP—supportive in short bursts but harmful if prolonged—has become a central focus in understanding how cellular senescence might contribute to regeneration rather than degeneration.
The timing and control of SASP release could be the secret to harnessing cellular senescence for healing purposes.
Why the Meniscus Struggles to Heal Naturally
The Meniscus Structure and Its Healing Limitations
The meniscus is critical for knee function. It absorbs shock, distributes body weight, and stabilises the joint during movement.
Its structure consists of a well-vascularised outer zone, which can heal naturally due to its blood supply, and an inner avascular zone, which lacks blood vessels and struggles to regenerate after injury. Tears in the inner meniscus often don’t heal well on their own and require medical interventions.
Conventional treatments, including surgery, are limited by the meniscus' unique structure. While surgery can help alleviate symptoms, it doesn’t always restore full function, and the lack of self-repair capability in the inner meniscus remains a challenge.
This has led researchers to look into alternative strategies, including leveraging the body’s natural healing processes, which brings us back to the potential role of cellular senescence and SASP in regeneration.
Cellular Senescence and Meniscus Repair in Rats
Senescent Cells in Meniscus Healing
The research team led by Yusuke Aimono and colleagues sought to understand whether cellular senescence contributes to the self-repair of the rat meniscus.
Using a partial medial meniscectomy (pMx) model, where a section of the rat’s meniscus was removed, they created a setup to observe tissue regeneration over time. By examining cellular senescence markers and SASP activity in the regenerating tissue, they aimed to uncover if and how senescent cells play a role in spontaneous meniscus repair.
Key Findings
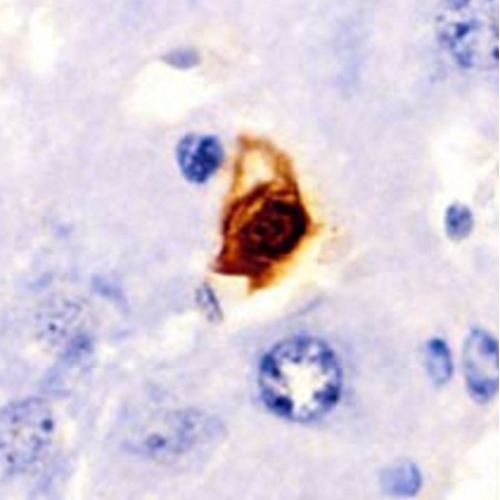
The study found significant increases in markers of cellular senescence, including p16—a well-established indicator of senescent cells—in the regenerating meniscus tissue, especially in the early stages after surgery.
Additionally, the presence of senescence-associated beta-galactosidase (SA-β-gal), another hallmark of cellular senescence, confirmed that these senescent cells were accumulating in the regenerating tissue. This early accumulation of senescent cells seemed to signal the onset of a repair process, suggesting that their presence may stimulate or support regeneration.
The SASP produced by senescent cells had a key role in meniscus repair. It appeared that the SASP factors prompted the proliferation of nearby cells, including synovial fibroblasts, which have the potential to differentiate and aid in tissue repair. In essence, senescent cells and their secreted factors were positively impacting the healing process in the rat meniscus, initiating a cascade of events that led to tissue regeneration.
SASP’s Effect on Synovial Fibroblasts
Synovial Fibroblasts: A Key Component in Meniscus Regeneration
Synovial fibroblasts (SFs) are specialised cells located in the knee joint synovium, a membrane that lines the joint and produces synovial fluid for lubrication.
In this study, SASP factors released by senescent cells appeared to have a stimulating effect on synovial fibroblasts, encouraging them to proliferate and possibly transform into cells that support cartilage formation.
In Vitro Findings: Boosting Repair-Related Genes
To explore SASP’s effect further, the researchers conducted in vitro experiments exposing normal SFs to conditioned medium (CM) containing SASP factors from senescent SFs.
Results showed that SFs exposed to SASP-rich medium displayed increased proliferation and signs of chondrogenic differentiation, which is the process of forming cartilage-like cells. Key genes associated with cartilage repair, including SOX9, a master regulator of cartilage formation, were highly expressed in SFs treated with SASP factors.
This strongly suggests that SASP can stimulate the necessary cellular changes to support meniscus repair, making SASP a potential target for regenerative therapies.
Testing Senolytic Drug ABT-263 in Meniscus Repair
Senolytics: A Double-Edged Approach
Senolytics are drugs that selectively eliminate senescent cells. The idea is that removing these cells may reduce inflammation and improve tissue function, especially in ageing or degenerative conditions.
However, given the positive role of senescent cells in meniscus regeneration, the researchers hypothesized that removing them too early might negatively impact repair.
The Role of ABT-263 in Meniscus Healing
To test this, the team administered ABT-263 to rats following their meniscus surgery. This drug selectively targets and removes senescent cells, including those with active SASP production. Interestingly, results showed that eliminating senescent cells with ABT-263 actually slowed down the healing process.
Regenerated tissues in the ABT-263-treated group had a less organized structure, lower levels of cartilage-like cells, and reduced expression of essential markers such as SOX9 and collagen. These findings underscore the importance of allowing a temporary presence of senescent cells, as their removal can disrupt the regenerative effects of SASP.
Implications for Therapy
This part of the study highlights a crucial insight: senescent cells and their SASP factors may be beneficial for meniscus healing when allowed to act for a limited period.
The transient presence of senescent cells seems essential for initiating tissue repair, but prolonged accumulation could lead to inflammation and degradation. Therefore, timing might be key in future therapeutic approaches that involve cellular senescence.
Future of Meniscus Regeneration and Cellular Senescence
Leveraging Cellular Senescence for Joint Repair
The study suggests an intriguing possibility for the future of meniscus repair: using cellular senescence as a tool rather than an obstacle. Instead of relying solely on surgical options, researchers could develop therapies that encourage controlled senescence in targeted areas, harnessing the benefits of SASP without risking prolonged inflammation.
For example, treatments could involve the temporary induction of senescent cells in the injury site or directly administering SASP-like factors to stimulate the repair process.
Challenges and Considerations
Although promising, the application of senescence-based therapies poses challenges. The transient nature of senescent cells' beneficial effects must be carefully controlled.
Too few senescent cells may hinder repair, while too many could lead to tissue damage. Researchers need to develop strategies that balance these factors, possibly through controlled drug delivery systems or precise timing in therapy administration.
Broader Applications
While this study focused on the rat meniscus, the findings have broader implications. Cellular senescence may support regeneration in other tissues and could influence treatments for various age-related conditions.
If senescent cells can facilitate natural repair mechanisms, their applications in regenerative medicine could be vast, extending to cartilage repair, wound healing, and even heart repair.
Conclusion
The study on cellular senescence and meniscus repair in rats presents exciting possibilities for regenerative medicine. By examining the role of senescent cells and their SASP factors, researchers have uncovered a potential pathway to encourage natural healing in damaged tissues. This study shifts the perspective on cellular senescence, traditionally seen as a barrier to healthy ageing, by highlighting its dual role in both repair and degeneration.
For now, further research is needed to determine how best to harness these insights for human treatments. However, the findings lay the groundwork for innovative therapies that leverage the body’s own biological mechanisms, turning the challenges of cellular ageing into opportunities for healing and regeneration.
The study is published in the journal Aging Cell. It was led by Ichiro Sekiya from Tokyo Medical and Dental University (TMDU).