A Silent Fire: The Story of Inflammation, Diet, and Disease
A riveting investigation of inflammation written by gastroenterologist Shilpa Ravella
Inflammation is the body’s ancestral response to its greatest threats, the first line of defense it deploys against injury and foreign pathogens. But as the threats we face have evolved, new science is uncovering how inflammation may also turn against us, simmering underneath the surface of leading killers from heart disease and cancer to depression, aging, and mysterious autoimmune conditions.
In A Silent Fire, gastroenterologist Shilpa Ravella investigates hidden inflammation’s emerging role as a common root of modern disease—and how we can control it. We meet the visionary nineteenth-century pathologist who laid the foundation for our modern understanding of inflammation, the eccentric Russian zoologist who discovered one of the cells central to our immune system, and the dedicated researchers advancing the frontiers of medical and nutritional science today. With fascinating case studies, Ravella reveals how we can reform our relationships with food and our microbiomes to benefit our own health and the planet’s.
A Silent Fire Book Review
The chapter titles for this book (including such delights as Horror Autotoxicus, A Sense of Strangling, Fat Wars and Dirty Cures) sum up Shilpa Ravella's style for telling the reader about the fascinating history of inflammation and what we know about it today. The language is image provoking and pleasing to read, even when it gets slightly heavy going as she delves into some of the biological detail. The personal experiences retold also help portray the emotion of the author.
I always enjoy a history of medicine book, as it shows how we got to our current knowledge - not in one big eureka moment, but in many small steps (some taken in the wrong direction) amidst personal and political shenanigans - and also provides a deeper understanding of the subject by following the thought processes taken over hundreds of years. Even if the big conclusion is (spoiler alert!) ... inflammation is bad for you.
Highlights
Here are 101 key points from A Silent Fire:
- Inflammation is an ancestral response that evolved to protect the body from threats and contain damage, be it from a microbe, chemical, or trauma.
- In the 1850s, German scientist Rudolf Virchow became the first to identify the cellular characteristics of inflammation.
- Doctors name what they see, often using the suffix -itis to denote inflammation.
- Hidden inflammation can be both a consequence and a cause of disease.
- Nearly five thousand years ago, writings on Egyptian papyri pointed to heat and redness as markers of disease.
- The immune system gives rise to diverse types of inflammation — acute or chronic, overt or obscure.
- In the late 19th century, stemming from only a few early experiments, Metchnikof had come up with the concept of an immune system.
- Acute inflammation comes and leaves quickly, typically in a few days.
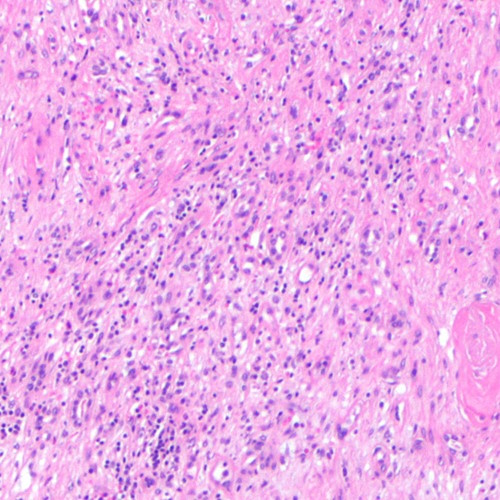
- While neutrophils and — to a lesser extent — macrophages are found in acute inflammation, macrophages and lymphocytes predominate in chronic inflammation.
- Paroxysmal cold hemoglobinuria, was the first discovery of an autoimmune disease in human beings.
- The 2011 Nobel Prize celebrated the essential, interwoven roles of both innate and adaptive immune responses.
- Inflammation is involved not only in a few select disorders but in a wide range of ailments that are the most common causes of death in the world today.
- Libby discovered that the cytokine interleukin 1 beta (IL-1β) had one of the strongest stimulatory effects on endothelial cells.
- Most heart attacks and many strokes happen after the fibrous cap of an inflamed atherosclerotic plaque burst open.
- LDL-mediated injury transforms endothelial cells much like cytokines do, disabling their original function and turning them into inflammatory powerhouses.
- Inflammation begets blood clots, and blood clots amplify inflammation.
- Smokers have elevated levels of inflammatory markers in the blood.
- A quarter of heart attacks and strokes did not have any cardiovascular risk factors at all, including hypertension, diabetes, obesity, or a history of smoking.
- Barring a serious inflammatory event like infection or trauma in the few weeks before a sample is taken, CRP levels tend to be stable in blood for decades.
- Otherwise healthy men in their forties with the highest CRP levels are three times as likely to suffer a heart attack and twice as likely to have a stroke over the next few years over men with little or no chronic inflammation.
- CRP is the downstream result of innate immune activation, produced in the liver when inflamed areas of the body release cytokines.
- IL-6 is increased decades in advance of heart disease.
- CRP is an independent risk factor for cardiovascular events, distinct from LDL cholesterol or other risk factors.
- In 2001, JUPITER trial patients with high CRP and low cholesterol levels who had gotten statins lowered their risk of having a heart attack or stroke by 44 percent.
- People with gene variants that blunt IL-6 activity and thereby systemic inflammation have a lower risk of heart disease.
- CANTOS trial provided hard evidence that solely intervening on inflammation could improve outcomes in heart disease patients, that inflammation was a cause of heart disease.
- Growing evidence shows that colchicine also lowers the risk of adverse cardiac events in people with heart disease.
- Rudolf Virchow was one of the first physicians to point out that cancer and inflammation were intricately linked.
- When Frances Balkwill turned off the TNF-α gene in mice, eradicating even low levels of TNF-α activity, the mice did not develop tumors.
- The immune cells that secrete growth factors to repair tissue in a wound serve to fuel a tumor’s uncontrolled proliferation.
- Celiac disease patients who fail to strictly avoid gluten may have ongoing intestinal inflammation, increasing their risk for several types of intestinal cancers.
- Even severe inflammation of the joints or brain carries little increased cancer risk.
- Studies also show that elevated markers of hidden inflammation, like CRP, are tied to a higher risk of some cancers and predict worse survival.
- Fat is an organ involved in controlling metabolic processes.
- Macrophages lodged in the fat of mice and humans are responsible for most of the inflammatory cytokines coming from fat tissue.
- The number of macrophages in the fat of mice and humans is over 50 percent in the markedly obese.
- Macrophages and adipocytes derive from the same ancestral cell in our evolutionary past.
- Visceral fat is highly inflammatory, hosting the most macrophages and spewing out an array of cytokines.
- The hallmarks of ageing are not independent entities but highly interconnected processes, converging on inflammaging, radiating through it like spokes on a wheel.
- When the kidneys malfunction, the body builds up inflammatory triggers, including waste material.
- Osteoarthritis, once thought to be a simple “wear and tear” joint disease, is now known to be, in part, an inflammatory one.
- Microglia, the most numerous cells in our brains aside from neurons, are central to the link between inflammation and neurodegeneration.
- Macrophages and cytokines can cross the blood-brain barrier or relay inflammatory signals through the endothelial cells.
- An inflamed body in middle age, in one’s forties and fifties, maybe even earlier, is linked to mental decline in later years.
- Inflammation is both a cause and a consequence of many strokes.
- Inflammation may affect not only physical health but also mental health, including depression, suicide, anxiety, post-traumatic stress disorder, schizophrenia, bipolar disorder, and autism.
- Hidden inflammation is one important mechanistic link between many environmental triggers and the ailments they are associated with.
- The gastrointestinal tract has a surface area much larger than that of the skin.
- The intestines contain the largest reservoir of macrophages in the body.
- Transplanting gut microbes — as one would transplant an organ — can alter the recipient’s microbiome and calm intestinal inflammation.
- Microbes from fat and thin human twins infused into skinny, germ-free mice resulted in the mice that received the fat twin’s microbes becoming fat.
- A dysbiotic microbiome is very often an inflammatory microbiome.
- A human hand harbors over a hundred different bacterial species, only a few of which are common to both hands.
- Studies do reveal a vague yet defining characteristic of healthy microbiomes: a richness, or diversity, of species.
- In most parts of the Mediterranean, 15 to 20 percent of a person’s daily calories came from olives and olive oil.
- Saturated fats activate NF-κB, stimulating inflammatory molecules like IL-6, CRP, and TNF-α.
- A growing body of research emphasizes the importance of omega-3s in an array of chronic inflammatory diseases.
- Since they grow rancid more readily than other types of fats, plant breeders often select for crops with fewer omega-3s.
- Many studies have shown that trans fats are tied to chronic, low-level inflammation.
- By June of 2015, the FDA finally ruled that trans fats were no longer “Generally Recognized as Safe (GRAS)” and called for their complete removal from the food supply.
- A large load of salt sends macrophages into turmoil, driving them to assemble NLRP3 and other inflammasomes.
- Salt disables Tregs, the regulatory white blood cells that are critical for balancing inflammation.
- Hidden inflammation is implicated in arterial stiffening, and hypertensive patients have increased levels of inflammatory molecules in their blood.
- Dental diseases like gingivitis — inflammation of the gums — can lead to hidden inflammation throughout the body.
- Excess sugar and other refined carbohydrates, robbed of nutrients but replete in calories, are tied to hidden inflammation and chronic inflammatory diseases.
- One of the main culprits in cultivating an inflammatory microbiome is an overload of modern animal fare.
- Animal protein helps to create an inflammatory microbiome that fosters disease, while plant protein has the opposite effect.
- Heme iron has been linked to a variety of chronic inflammatory diseases.
- Diets high in fiber are tied to lower levels of inflammatory markers— including CRP, IL-6, and TNF-α— in specific tissues and throughout the body even after controlling for weight.
- Short-chain fatty acids can influence immune function in ways that hamper hidden inflammation and chronic inflammatory diseases.
- Surplus of secondary bile acids promotes inflammatory microbes and adversely affects immune cells and inflammation.
- Artificial sweeteners induce changes in the gut microbiome that promote inflammation and insulin resistance.
- Emulsifiers like polysorbate-80 and maltodextrin help invasive microbes thought to play a part in inflammatory bowel disease tunnel through the gut wall.
- The Western diet is tied to altered expression of inflammatory genes and high blood levels of inflammatory markers.
- Vitamin D deficiency is tied to many chronic inflammatory diseases.
- Many phytochemicals benefit human health, uniquely affecting germs, inflammation, and disease.
- Aryl hydrocarbon receptor expression is decreased in inflammatory bowel disease patients.
- Okinawans subsisted largely on leafy greens, root vegetables, legumes, whole soy foods, and whole grains.
- Sweet potatoes are rich in nutrients that manage inflammation and enhance immunity.
- Amla (indian gooseberry) is packed with polyphenols and has two hundred times the antioxidant capacity of blueberries.
- Ginger bolsters immunity and combats inflammation.
- Curcumin inhibits many inflammatory pathways, including some targeted by major anti-inflammatory drugs.
- Overwhelming evidence for the following hypothesis: a diverse diet made up largely or entirely of whole plant foods is the best way of eating to prevent— or, in many cases, to treat— most chronic inflammatory diseases that plague modern humankind.
- Severe stress may muffle the beneficial effects of an anti-inflammatory diet.
- Human clinical trials indicate that tomatoes increase immunity and reduce low-level inflammation in the body.
- After an identical meal, levels of inflammation can vary significantly between healthy adults.
- Lactic acid directly decreases inflammation in the gut and prevents macrophages from secreting inflammatory cytokines.
- Probiotic supplements can have anti-inflammatory effects, but they may be best used in disease rather than in health at present.
- Ancient grains may suppress inflammation more easily than their modern counterparts.
- People with non-celiac wheat sensitivity tend to have low-level intestinal inflammation and a robust rise in markers of innate immune inflammation and intestinal damage floating in the blood.
- For the vast majority of the population, gluten-containing whole grains help to prevent or treat chronic inflammatory diseases.
- Produce grown with fewer pesticides build up more polyphenols as well as salicylic acid.
- The diversity of species in the human microbiome, a marker of its health, has been steadily shrinking over time, particularly since the Industrial Revolution.
- When children are exposed to greater numbers of microbes during infancy, their risk of hidden, chronic inflammation in adulthood may decrease.
- Blue zone dwellers consume a diet of around 95 to 100 percent whole plant foods.
- Dozens of human clinical trials across age-groups show that regular exercise tones down chronic, low-level inflammation.
- Stressful situations— even ostensibly moderate ones, like public speaking— are tied to a rise in blood markers of inflammation.
- Sleep loss, a type of chronic stress, can feed hidden inflammation and disease.
- Chronic exposure to air pollution is linked to elevated levels of inflammatory markers.
- In an infectious viral illness, the line between helpful and harmful inflammation can be blurry and hard to define.
- Chronic, low-level inflammation can impair the immune system’s ability to store intelligence about past encounters with pathogens.
Visit website: https://shilparavella.com/category/books/
Shilpa Ravella
Assistant Professor of Medicine at Columbia University Medical Center, gastroenterologist and author
Details last updated 21-Feb-2025