Ageing is a natural process, but it often brings various age-related diseases, especially cardiometabolic ones like heart disease, diabetes, and metabolic syndrome. At the heart of these diseases lies cellular senescence, a phenomenon where cells permanently stop dividing. While senescence helps prevent cancer by stopping cells with damaged DNA from growing uncontrollably, it also has a dark side. As senescent cells accumulate, they release inflammatory molecules that impact neighboring healthy cells, leading to chronic inflammation and tissue damage. Understanding and controlling cellular senescence holds the potential to combat cardiometabolic diseases and promote healthier ageing.
What is Cellular Senescence?
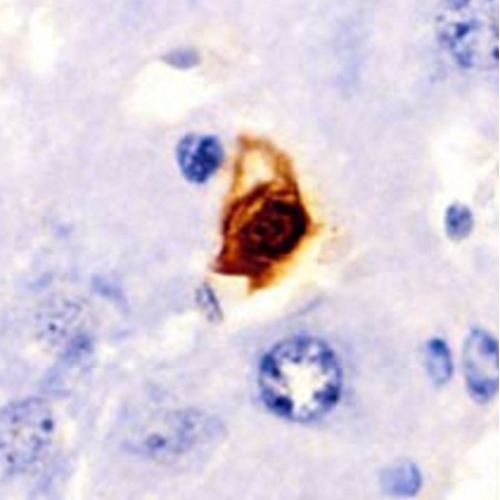
Cellular senescence is a complex biological process where cells enter a state of permanent growth arrest. Unlike normal cells that can divide, senescent cells are non-dividing yet metabolically active. They exhibit specific markers, like senescence-associated beta-galactosidase (SA-β-Gal), and express proteins that prevent cell division, such as p16 and p21.
Senescent cells contribute to ageing by releasing a mix of pro-inflammatory signals known as the senescence-associated secretory phenotype (SASP). SASP includes cytokines, chemokines, and proteases that can disrupt tissue structure and function. While SASP can support healing by signaling immune cells, its prolonged presence can cause chronic inflammation, leading to age-related diseases, particularly in cardiovascular and metabolic systems.
Mechanisms Triggering Cellular Senescence
Cellular senescence can be induced by several triggers:
DNA Damage: Chronic DNA damage from environmental factors like radiation, oxidative stress, or even ageing leads cells to stop dividing to prevent mutation spread.
Oxidative Stress: Reactive oxygen species (ROS) accumulate in cells with age, damaging DNA, proteins, and lipids. This ongoing stress can push cells into senescence, causing them to release more ROS, creating a damaging feedback loop.
Telomere Shortening: With each cell division, the protective caps on chromosomes, called telomeres, shorten. Once they reach a critical length, cells enter senescence as a preventive measure against genetic instability.
Metabolic Changes: Metabolic shifts in ageing cells, like reduced NAD+ levels and increased fatty acid oxidation, contribute to senescence by altering the cell’s energy state.
Each of these mechanisms is crucial in the progression of cardiometabolic diseases.
Senescence in Cardiometabolic Diseases
Cellular senescence has a significant impact on cardiometabolic diseases, such as:
1. Atherosclerosis
Atherosclerosis, the buildup of plaques in arteries, is a leading cause of heart disease. Studies show that senescent cells in blood vessel walls release SASP factors, leading to inflammation and plaque instability. The accumulation of senescent cells in plaques drives disease progression and can lead to events like heart attacks. Current research shows that eliminating senescent cells in animal models reduces plaque formation, pointing to senolytic drugs as a promising intervention.
2. Heart Failure and Cardiac Ageing
Heart failure, especially heart failure with preserved ejection fraction (HFpEF), is commonly seen in older adults. As heart cells age, they accumulate damage and undergo senescence, contributing to stiffness and impaired heart function. In HFpEF, senescent cells, particularly in the heart's endothelial cells, promote inflammation and fibrosis, worsening cardiac health. Therapeutic interventions targeting senescence in these cells have shown improved heart function in experimental studies.
3. Metabolic Syndrome and Diabetes
Metabolic syndrome, a cluster of conditions like obesity and high blood pressure, often leads to diabetes and cardiovascular diseases. Senescent cells accumulate in fat tissue, liver, and pancreatic beta cells in these conditions, releasing SASP factors that drive inflammation and insulin resistance. Studies show that removing senescent cells can improve glucose tolerance and insulin sensitivity, offering hope for treating metabolic syndrome and diabetes through senescence-targeted therapies.
4. Diabetic Cardiomyopathy
Diabetes increases the risk of heart disease through diabetic cardiomyopathy (DCM), where the heart’s structure and function deteriorate. In DCM, senescent cells in cardiac tissue contribute to chronic inflammation, mitochondrial dysfunction, and insulin resistance, impairing heart function. Targeting senescence in cardiac cells may offer a way to treat or prevent DCM, supporting the heart’s resilience against diabetic damage.
Therapeutic Approaches to Combat Senescence
Researchers are exploring therapies that either remove senescent cells or reduce their harmful effects:
Senolytics
These drugs selectively eliminate senescent cells by inducing apoptosis (programmed cell death). Dasatinib and Quercetin (D+Q) are senolytics shown to be effective in various disease models. D+Q reduces senescent cell burden in fat tissue, improves glucose metabolism, and alleviates insulin resistance. ABT-263, another senolytic, has shown promise in reducing senescent cell accumulation in heart tissue, enhancing cardiac function in animal models. However, senolytics must be used carefully due to potential side effects like immunosuppression.
Senostatics
Unlike senolytics, senostatics inhibit the harmful SASP without killing the cells. Drugs like rapamycin, metformin, and resveratrol fall into this category, helping reduce inflammation and metabolic dysfunction. Rapamycin, for instance, targets the mTOR pathway, which regulates cell growth and SASP production. Senostatics offer a safer alternative to senolytics, but research is still ongoing to optimize their efficacy.
Immunosurveillance and Senescence Vaccines
Enhancing the immune system’s ability to clear senescent cells is another promising approach. Some therapies under study involve using CAR-T cells (genetically engineered immune cells) to target senescent cells, while others explore vaccines that train the immune system to recognize and eliminate senescent cells. These immunotherapies hold the potential to prevent senescent cells from accumulating, but they also face challenges like immunosenescence, where the immune system itself ages.
Metabolic Modulators
Metabolic modulators like NAD+ precursors and sirtuin activators have shown promise in restoring cellular energy balance, reducing oxidative stress, and delaying senescence. NAD+ boosters, such as nicotinamide mononucleotide (NMN), improve mitochondrial function and have anti-senescence effects in animal studies. This approach aims to reverse cellular ageing at the metabolic level, offering a complementary therapy to senolytics and senostatics.
Challenges and Future Directions
While anti-senescence therapies show great promise, several challenges remain. First, a lack of specific markers for senescent cells limits our ability to identify and target them accurately. Most markers used today, like p16 and SA-β-Gal, can be present in non-senescent cells, leading to potential off-target effects. Moreover, since senescent cells play roles in wound healing and tissue repair, eliminating them indiscriminately could disrupt these beneficial processes.
Long-term safety is also a concern. Senolytic drugs like ABT-263 can reduce platelet counts, increasing bleeding risk. Similarly, Dasatinib can impact immune cells, leading to possible immunosuppression. Future research needs to focus on developing senolytics with fewer side effects or using them in lower, intermittent doses to minimize risks.
A promising avenue is the development of senescence-specific vaccines and CAR-T cell therapies. By targeting surface proteins unique to senescent cells, these therapies could selectively remove senescent cells without affecting healthy tissues. Combining senolytics with immunotherapies might yield the best results for complex cardiometabolic conditions.
Path Forward
The study of cellular senescence has transformed our understanding of ageing and age-related diseases. Cardiometabolic diseases, driven by the accumulation of senescent cells and chronic inflammation, may one day be treatable through senescence-targeted therapies. Senolytics, senostatics, metabolic modulators, and immunotherapies offer promising pathways to manage or even prevent diseases like atherosclerosis, heart failure, diabetes, and diabetic cardiomyopathy.
However, researchers must overcome challenges in safety, specificity, and understanding senescence’s complex roles. As our knowledge grows, these therapies could reshape how we approach ageing and age-related diseases, helping individuals lead healthier, longer lives.
The study is published in the journal Npj Aging. It was led by Mandy O. J. Grootaert from UCLouvain, Brussels.