Key points from article :
Researchers at The Ohio State University have developed a groundbreaking light-based gene therapy, called mLumiOpto, that disrupts cancer cells’ energy-producing mitochondria, triggering their destruction. This innovative approach uses nanoparticles to deliver gene therapy specifically to cancer cells, and experiments in mice have demonstrated its effectiveness in shrinking glioblastoma brain tumours and aggressive triple-negative breast cancer tumours. The study, published in Cancer Research, was co-led by Dr. Lufang Zhou, a professor of biomedical engineering and surgery, and Dr. X. Margaret Liu, a professor of chemical and biomolecular engineering.
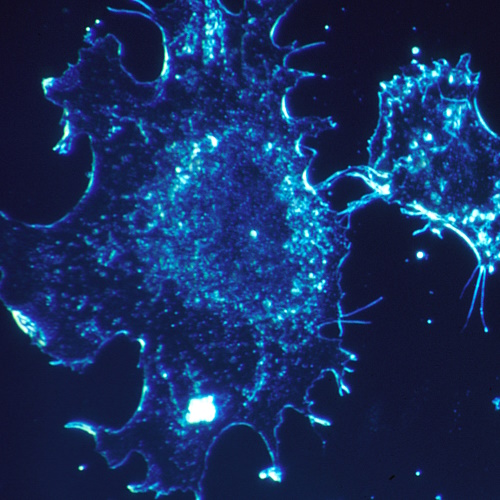
Mitochondria, often called the "powerhouses" of cells, have long been seen as promising targets for cancer therapy, but their impermeable inner membrane has made them challenging to disrupt. The mLumiOpto technique addresses this by delivering genetic instructions for two key proteins: a light-sensitive protein that generates electrical currents and an enzyme that emits bioluminescent light. Once inside the mitochondria of cancer cells, these proteins are activated by a chemical injection, creating light-driven electrical currents that destabilize the mitochondria, leading to cancer cell death while sparing healthy cells.
Dr. Liu’s lab designed a highly targeted delivery system using an engineered virus coated in natural nanocarriers derived from human cells. This ensures stability and precise targeting, enhanced further by attaching a monoclonal antibody that recognizes receptors on cancer cell surfaces. This dual strategy not only disrupts cancer cells but also appears to stimulate the immune system to attack remaining tumour cells.
Mouse studies showed significant tumour reduction and improved survival in glioblastoma and triple-negative breast cancer models, with no damage to healthy tissue. The researchers are now exploring additional applications of mLumiOpto and have filed a provisional patent for this promising technology. If successful in further studies, this approach could represent a major advancement in treating difficult-to-target cancers.