Have you ever wondered how your gut and bones are connected? Recent research shows a fascinating link between the bacteria in our guts and the stem cells in our bone marrow. This connection, known as the gut-bone marrow axis, plays a crucial role in our health, especially as we age. Let's dive into how this relationship works and why it matters to you.
Gut microbiome
Our gut is home to a bustling community of bacteria, fungi, and viruses, collectively known as the gut microbiome. These tiny organisms help us digest food, fight off infections, and even influence our mood.
Components of the Gut Microbiome
Our gut is packed with trillions of microorganisms. Key players include bacteria like Bacteroides and Firmicutes, which aid in digestion and support our immune system.
However, the gut microbiome isn't static; it changes as we grow. Babies inherit their first microbes from their mothers during birth and breastfeeding. As we age, our diet, lifestyle, and medications shape our gut flora. In our later years, the diversity of these microorganisms tends to decrease, which can affect our health.
Ageing and the Gut: What Happens?
As we age, our gut microbiome undergoes significant changes.
Microbiome Diversity
Research shows that older adults often have a less diverse gut microbiome. This decline in diversity can contribute to various health issues, including increased inflammation and a weaker immune system.
Impact of Diet and Lifestyle
What we eat and how we live play crucial roles in shaping our gut health. For instance, a high-fiber diet can promote a healthy gut, while a diet high in processed foods can harm it. Frequent use of antibiotics can also disrupt the balance of our gut bacteria.
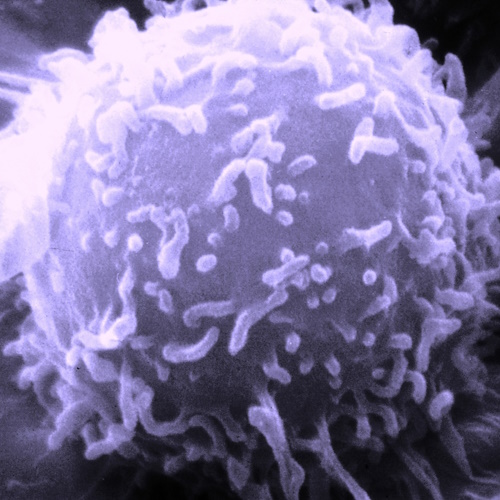
Hematopoietic Stem Cells (HSCs)
Hematopoietic stem cells are vital for producing blood and immune cells. These stem cells reside in our bone marrow and have the remarkable ability to renew themselves and differentiate into various types of blood cells.
HSCs are the body's builders, ensuring a steady supply of red blood cells, white blood cells, and platelets. These cells are essential for carrying oxygen, fighting infections, and clotting blood.
As we age, our HSCs become less efficient. They tend to produce more myeloid cells, which can lead to a weakened immune system. This shift makes older adults more susceptible to infections and blood disorders.
The Gut-Bone Marrow Connection: How It Works
The gut microbiome and the hematopoietic system are interconnected through the gut-bone marrow axis. This relationship is mediated by various molecules produced by gut bacteria, such as short-chain fatty acids (SCFAs), lactate, and indole.
Key Mediators:
- SCFAs: These fatty acids, including acetate, butyrate, and propionate, are produced by the fermentation of dietary fibers. They help maintain gut health and regulate immune responses.
- Lactate: Produced by certain gut bacteria, lactate influences HSC differentiation and supports the production of new blood cells.
- Indole: A metabolite derived from tryptophan, indole helps maintain gut barrier integrity and modulates immune responses.
These molecules can enter the bloodstream and travel to the bone marrow, where they interact with HSCs, influencing their behavior and function. For example, butyrate has been shown to enhance HSC activity by increasing local iron availability, crucial for blood cell production.
Inflammation and Ageing: The Microbiome’s Role
Chronic low-grade inflammation, or inflamm-ageing, is a hallmark of ageing. The gut microbiome plays a pivotal role in this process.
- Dysbiosis and Inflammation: An imbalanced gut microbiome can trigger inflammatory pathways. Dysbiosis, characterized by a reduction in beneficial bacteria and an increase in harmful ones, leads to increased production of pro-inflammatory cytokines. These cytokines can affect HSCs, contributing to age-related decline in immune function.
- Impact on HSC Regulation: Chronic inflammation influences HSCs, reducing their ability to regenerate and function effectively. This can result in a less responsive immune system and increased vulnerability to diseases.
Blood Disorders and the Microbiome: A Deep Dive
The gut microbiome significantly impacts the risk and progression of hematologic disorders.
Leukemia and Gut Health: In leukemia patients, maintaining a healthy gut microbiome can improve treatment outcomes. Studies have shown that patients with diverse gut flora respond better to chemotherapy. Antibiotic treatments, often used to prevent infections in these patients, can disrupt gut health, highlighting the need for balanced microbial communities.
Other Blood Disorders: Conditions like anemia and myelodysplastic syndromes (MDS) also show links to gut health. Dysbiosis can exacerbate these conditions by affecting iron absorption and inflammatory responses.
Research also indicates that individuals with a healthier gut microbiome have a lower incidence of hematologic disorders. For example, a study found that patients with higher microbial diversity had better survival rates in multiple myeloma.
Looking Forward
Emerging research suggests that manipulating the gut microbiome could offer new therapeutic avenues.
Probiotics and Prebiotics: Supplementing the diet with probiotics (beneficial bacteria) and prebiotics (compounds that promote the growth of beneficial bacteria) can help restore and maintain a healthy gut microbiome. These interventions show promise in supporting HSC function and reducing inflammation.
Fecal Microbiota Transplants (FMT): This procedure involves transferring stool from a healthy donor to a patient with dysbiosis. FMT has shown success in treating conditions like Clostridium difficile infection and is being explored for its potential in improving outcomes in hematologic disorders.
Scientists are investigating the specific mechanisms by which gut bacteria influence HSCs and the immune system. Understanding these pathways could lead to targeted therapies that enhance gut health and, in turn, improve overall health and longevity.
The relationship between the gut microbiome and the hematopoietic system is crucial for maintaining health, especially as we age. By unraveling the complexities of the gut-bone marrow axis, researchers can develop targeted interventions to enhance immune function and mitigate the effects of ageing on blood health.
The future holds promising possibilities for harnessing the power of the microbiome to improve overall health and well-being.
Understanding this link will also lead to highlighting mechanisms associated with disease onset and whether the supplementation of particular microbiota and or factors may offer an alternative route of prevention against hematologic diseases.
The study was led by Christopher Wells from the Queen's University and is published in the journal Heliyon.