The world's ageing population is facing an increasing prevalence of eye diseases like dry eye, cataract, glaucoma, and macular degeneration. Understanding the ageing process in the human eye, particularly the ocular surface composed of the cornea, conjunctiva, and tear fluid, is crucial. Past studies have linked ageing with chronic inflammation, characterised by the accumulation of senescent cells—cells that have stopped dividing and exhibit a pro-inflammatory state, known as the senescence-associated secretory phenotype (SASP).
The Role of Senescent Ocular Cells in Ageing Eyes
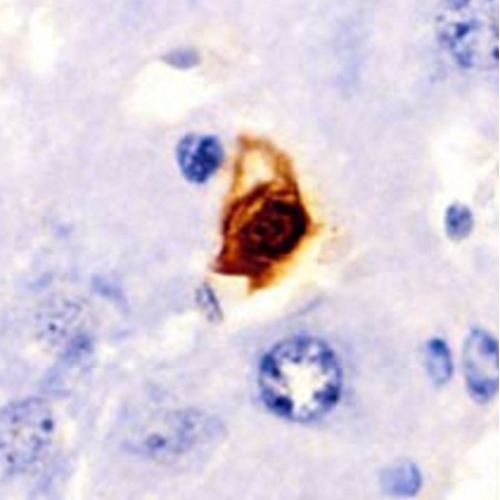
Recent breakthrough research led by the Buck Institute for Research on Ageing has made significant strides in understanding how senescent ocular cells (SOCs) contribute to age-related eye diseases. When human primary corneal epithelial cells were exposed to ionising radiation, a hallmark of DNA damage, they underwent senescence. This condition was marked by increased expression of senescent markers (like p16 and p21), a decrease in cell proliferation, and the secretion of pro-inflammatory factors part of SASP, such as IL-6, IL-1β, and various matrix metalloproteinases (MMPs). The presence of these factors suggests a link between SOCs and inflammation observed in ageing eyes.
Disruption of the Corneal Epithelial Barrier
One key finding of the study was how SOCs disrupt the corneal epithelial barrier, essential for maintaining clear vision. Experiments demonstrated that the transepithelial electrical resistance (TEER), a measure of barrier integrity, was significantly reduced in the presence of SOCs. Furthermore, treatment with a senolytic drug, ABT263, which selectively eliminates SOCs, restored TEER levels, underscoring the pivotal role of SOCs in compromising the ocular surface's barrier function.
Proteomic Analysis: Deciphering the SASP
A comprehensive proteomic analysis revealed a complex array of SASP components secreted by SOCs. The SASP is known for its diverse range of components, which vary depending on the cell type, physiological state, and environmental stimuli. The proteomic analysis in this study revealed a rich tapestry of factors, including inflammatory cytokines, chemokines, growth factors, and proteases. These components are crucial in understanding how SOCs contribute to the age-related deterioration of the ocular surface. The SASP factors secreted by SOCs play a significant role in driving the inflammatory processes observed in ageing eyes, impacting both the structure and function of the ocular surface.
The identification and characterisation of these SASP components provide valuable insights into how senescent cells influence the ageing eye. The presence of these factors could lead to chronic inflammation, disruption of the corneal epithelial barrier, and other age-related ocular changes. Understanding the specific components of the SASP in SOCs opens the door to targeted therapeutic strategies aimed at mitigating their detrimental effects. For instance, the study highlighted the potential roles of various matrix metalloproteinases (MMPs) and cytokines in maintaining the epithelial barrier function and influencing the health of the ocular surface.
Dry Eye Model in Mice
The research extended to animal models, where a dry eye (DE) condition was simulated in young and old mice through lacrimal gland excision (LGE). The study utilised both young (4 months old) and old (24 months old) mice to investigate the effects of ageing on the development of DE. The model was established through a procedure known as lacrimal gland excision (LGE), which is a well-recognised method for creating a condition of aqueous tear-deficient DE. LGE leads to tear film instability, a critical factor in all forms of DE. The procedure's impact was assessed by measuring tear fluid volume, which significantly decreased in LGE-treated eyes compared to sham eyes in both age groups.
One of the most striking findings was the difference in the response to LGE between young and old mice. While the young mice maintained corneal transparency post-LGE, the old mice exhibited pronounced corneal opacity accompanied by severe angiogenesis. This contrast underscores the vulnerability of the ageing ocular surface to stressors like tear deficiency. The aged mice also showed signs of corneal keratinisation, further highlighting the severe impact of DE in older subjects.
The DE mouse model provides a crucial platform for testing potential treatments and interventions for age-related ocular diseases. The observed differences between young and old mice open avenues for further research, particularly in developing strategies to prevent or treat the adverse effects of ageing on the eye. Given the study's focus on senolytic treatments, there is potential for translating these findings into therapies that target senescent cells to alleviate or prevent conditions like DE in the elderly.
A Ray of Hope
One of the most promising aspects of this study was the exploration of senolytic treatments. Application of topical ganciclovir (GCV) eye drops, which selectively remove senescent cells, showed that early intervention could prevent or mitigate corneal opacity and angiogenesis in aged mice suffering from DE. This suggests that reducing the burden of senescent cells on the ocular surface could be a potential therapeutic approach for age-related ocular diseases.
This study is a monumental step in understanding age-related ocular diseases. It underscores the critical role of cellular senescence in disrupting the epithelial barrier function and contributing to the development of diseases like DE. The findings suggest that senescent cells, through their SASP, not only drive chronic inflammation but also lead to physical changes in the eye, such as increased corneal opacity and reduced barrier function.
The potential of senolytic treatments offers a new avenue for therapeutic intervention, potentially revolutionising the management of age-related eye conditions.
Acknowledgements
This landmark study was conducted at the Buck Institute for Research on Aging. The findings of the research were published in the journal Aging Biology.