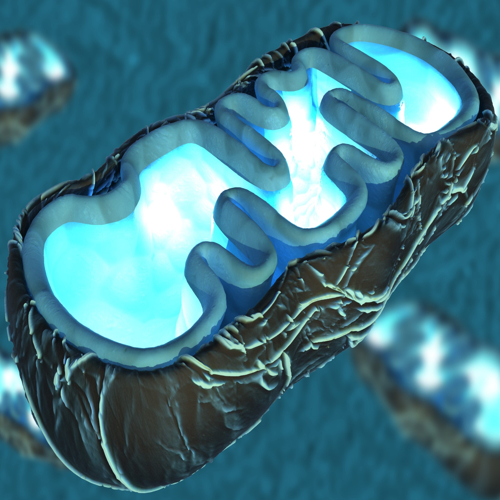
Ageing is an inevitable part of life, bringing with it changes that affect every organ in our body. Among all organs, the heart holds a unique significance due to its central role in maintaining health. One of the primary mechanisms by which ageing impacts heart function involves the tiny but mighty powerhouses of the cell – mitochondria.
These organelles are key to providing energy to the heart, and their dysfunction is closely tied to cardiac ageing and related health conditions. In this blog, we delve deep into the complex relationship between mitochondrial dysfunction and the ageing heart, exploring the mechanisms that cause bioenergetic decline, changes in cardiac structure, and the prospects for intervention.
The Ageing Heart
The process of ageing impacts the entire body, but it particularly affects the cardiovascular system, leading to changes in both the structure and function of the heart. As we age, the heart undergoes remodeling – a process involving changes in the size, shape, and function of heart tissues. These changes contribute to a gradual decline in heart function and increase susceptibility to diseases such as heart failure, hypertension, and arrhythmias.
But what are the drivers behind these changes? The mitochondria, often known as the energy producers of the cell, are at the center of this story. Ageing impacts mitochondrial function, which, in turn, impairs the heart's ability to maintain energy supply, adapt to stress, and carry out efficient contractile functions.
Mitochondrial Dysfunction and Bioenergetic Decline
Mitochondria play a crucial role in producing adenosine triphosphate (ATP), the energy currency that drives almost all cellular activities. In the heart, which requires a significant amount of energy to maintain continuous pumping, mitochondrial efficiency is vital for normal function.
The mitochondrial electron transport chain (ETC) is responsible for producing up to 90% of ATP in heart cells. Unfortunately, as we age, mitochondrial efficiency declines, leading to reduced ATP production and a subsequent energy deficit in cardiac cells.
The process of oxidative phosphorylation, which occurs within the mitochondria, becomes impaired in ageing. Components of the electron transport chain, such as Complex I and Complex IV, are particularly vulnerable to age-related changes.
This results in the leakage of electrons and the formation of reactive oxygen species (ROS) – highly reactive molecules that cause oxidative damage to proteins, lipids, and mitochondrial DNA (mtDNA). Elevated ROS levels contribute to further mitochondrial damage, reducing ATP production and triggering a vicious cycle of dysfunction.
Oxidative Stress and the Role of ROS
Oxidative stress is one of the main culprits behind mitochondrial dysfunction during ageing. Mitochondria are both the primary producers and targets of ROS. ROS are generated as by-products of the electron transport chain during ATP production.
In a young and healthy heart, antioxidant enzymes like superoxide dismutase (SOD), catalase, and glutathione peroxidase help neutralize ROS, maintaining a balance between their production and elimination. However, in ageing, this balance is disrupted, leading to oxidative stress.
Excessive ROS production damages the inner mitochondrial membrane, impairs ETC components, and causes mutations in mtDNA. The loss of mtDNA integrity further compromises mitochondrial function, as mtDNA encodes several essential proteins involved in ATP production.
Studies have shown that aged hearts have significantly increased levels of oxidative damage, including lipid peroxidation and oxidative modifications of mitochondrial proteins, which contribute to the decline in cardiac function.
Mitochondrial Dynamics: Fusion, Fission, and Mitophagy
Mitochondria are highly dynamic organelles that continuously undergo fusion (joining together) and fission (splitting apart). These processes are collectively known as mitochondrial dynamics and are essential for maintaining mitochondrial health.
Fusion helps mitigate stress by mixing the contents of partially damaged mitochondria, allowing for the repair of damaged components. Fission, on the other hand, facilitates the removal of damaged mitochondria through a process called mitophagy.
Ageing disrupts the balance between mitochondrial fusion and fission, leading to mitochondrial fragmentation and dysfunction. Key proteins involved in mitochondrial dynamics, such as mitofusins (MFN1 and MFN2) and dynamin-related protein 1 (Drp1), show altered expression in aged hearts.
Excessive fission results in smaller, fragmented mitochondria that are less efficient at producing ATP and more prone to generating ROS. Impaired fusion prevents the proper mixing of mitochondrial content, leading to the accumulation of damaged components.
Mitophagy, the selective degradation of damaged mitochondria, is another critical process that declines with age. The PINK1-Parkin pathway, which plays a central role in identifying and tagging damaged mitochondria for removal, becomes less effective in ageing. As a result, dysfunctional mitochondria accumulate, contributing to increased oxidative stress and reduced energy production.
Neurohormonal Systems and Cardiac Ageing
The ageing heart is also influenced by changes in neurohormonal systems, particularly the sympathetic nervous system and the renin-angiotensin-aldosterone system (RAAS). These systems play important roles in regulating cardiovascular function, including heart rate, contractility, and blood pressure. However, chronic activation of these systems during ageing leads to detrimental effects on the heart.
The adrenergic system, which involves the release of catecholamines like adrenaline and noradrenaline, becomes dysregulated in ageing. The sensitivity and density of beta-adrenergic receptors decline, leading to impaired cardiac response to stress. Chronic stimulation of beta-adrenergic receptors has been shown to induce mitochondrial dysfunction, contributing to mitochondrial membrane depolarization, increased ROS production, and apoptosis (programmed cell death) of cardiac cells.
Similarly, the RAAS becomes overactive with age, leading to increased levels of angiotensin II (Ang II). Ang II promotes the production of ROS, fibrosis (scarring of heart tissue), and inflammation, all of which contribute to the decline in cardiac function. Studies have shown that inhibiting RAAS using medications like enalapril or losartan can extend lifespan and delay age-related cardiovascular pathologies, highlighting the potential of targeting neurohormonal systems to mitigate cardiac ageing.
Calcium Handling and Mitochondrial-ER Crosstalk
Calcium ions (Ca2+) play a crucial role in cardiac function, acting as a signaling molecule that regulates muscle contraction and energy production. Mitochondria work closely with the sarcoplasmic reticulum (SR), a structure that stores and releases calcium, to maintain calcium homeostasis in cardiac cells. This close interaction between mitochondria and the SR, known as mitochondrial-ER crosstalk, is essential for efficient ATP production and contractile function.
In ageing, mitochondrial calcium handling becomes impaired, leading to disrupted energy production and increased susceptibility to stress. The physical and functional connection between mitochondria and the SR weakens, resulting in reduced calcium uptake by mitochondria. This affects the ability of mitochondria to produce ATP in response to increased energy demand.
Additionally, impaired calcium handling contributes to the opening of the mitochondrial permeability transition pore (mPTP), a channel that, when open, leads to cell death. The increased opening of mPTP in ageing hearts further exacerbates mitochondrial dysfunction and contributes to the loss of cardiac cells.
Fibrosis, Inflammation, and Cardiac Remodeling
Ageing is associated with an increase in fibrosis – the accumulation of excess extracellular matrix proteins, which leads to stiffening of the heart tissue. Fibrosis impairs the heart's ability to relax and fill with blood during diastole, contributing to diastolic dysfunction, a common feature of the ageing heart. Mitochondrial dysfunction plays a role in promoting fibrosis by increasing ROS production and activating pro-fibrotic signaling pathways, such as those involving transforming growth factor-beta (TGF-β) and matrix metalloproteinases (MMPs).
Chronic inflammation, often referred to as "inflammaging," is another hallmark of cardiac ageing. Mitochondrial ROS act as signaling molecules that activate pro-inflammatory pathways, leading to the release of cytokines and chemokines that promote inflammation. The activation of nuclear factor-kappa B (NF-κB), a key transcription factor involved in inflammation, is increased in ageing hearts. This chronic low-grade inflammation contributes to cardiac remodeling, fibrosis, and a decline in heart function.
Potential of Therapeutic Interventions
Given the central role of mitochondrial dysfunction in cardiac ageing, targeting mitochondria represents a promising therapeutic strategy for mitigating age-related cardiovascular decline. Several potential interventions are currently being explored to improve mitochondrial function and promote cardiac health in ageing populations.
1. Antioxidant Therapy:
One approach is to enhance the heart's antioxidant defenses to reduce oxidative stress. Mitochondria-targeted antioxidants, such as MitoQ and SkQ1, have shown promise in reducing ROS levels and improving mitochondrial function in preclinical studies. These antioxidants are designed to accumulate within mitochondria, where they can neutralize ROS and protect mitochondrial components from damage.
2. Caloric Restriction and Exercise
Lifestyle interventions, such as caloric restriction and regular exercise, have been shown to improve mitochondrial function and delay cardiac ageing. Caloric restriction reduces oxidative stress and promotes mitochondrial biogenesis – the production of new mitochondria. Exercise, particularly endurance training, enhances mitochondrial efficiency and increases the expression of proteins involved in mitochondrial dynamics and function.
3. Pharmacological Agents
Pharmacological agents that target mitochondrial dynamics and mitophagy are also being investigated. For example, drugs that activate the PINK1-Parkin pathway could enhance the removal of damaged mitochondria, improving mitochondrial quality control. Similarly, compounds that modulate the activity of proteins involved in mitochondrial fusion and fission could help restore the balance of mitochondrial dynamics in ageing hearts.
4. RAAS Inhibitors and Beta-Blockers
As discussed earlier, the RAAS and adrenergic systems contribute to mitochondrial dysfunction and cardiac ageing. Medications that inhibit these systems, such as angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), and beta-blockers, have been shown to improve mitochondrial function, reduce fibrosis, and delay the progression of heart failure in ageing individuals.
Protecting the Ageing Heart
The relationship between mitochondrial dysfunction and cardiac ageing is complex, involving a web of interconnected pathways that contribute to bioenergetic decline, oxidative stress, fibrosis, and inflammation.
As the heart ages, its ability to produce energy, respond to stress, and maintain efficient function is compromised, largely due to changes in mitochondrial health. However, the growing understanding of the mechanisms underlying mitochondrial dysfunction in ageing provides hope for developing targeted interventions that can improve cardiac health and extend lifespan.
Therapeutic strategies aimed at enhancing mitochondrial function, reducing oxidative stress, and improving mitochondrial quality control hold promise for mitigating the impact of ageing on the heart. Lifestyle interventions, such as regular exercise and caloric restriction, along with pharmacological approaches, offer potential avenues for preserving mitochondrial health and promoting cardiovascular well-being in older adults.
As research in this field continues to evolve, the prospect of maintaining a healthy heart well into old age becomes increasingly achievable. By targeting the root causes of mitochondrial dysfunction, we may one day be able to protect the heart from the ravages of time and ensure a healthier, more vibrant life for ageing individuals.
The study is published in The Journal of Cardiovascular Aging. It was led by Pasquale Mone from Albert Einstein College of Medicine, New York.