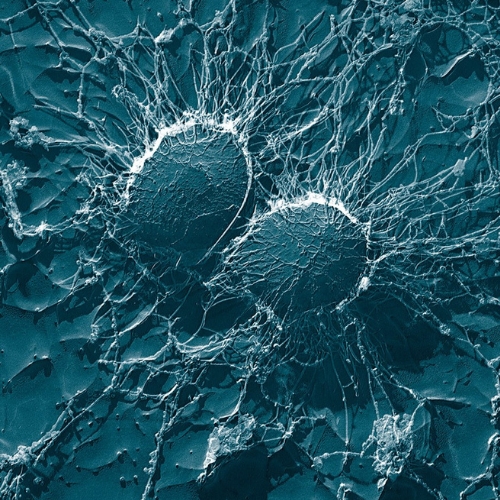
The human body hosts trillions of microorganisms, forming a complex ecosystem known as the microbiome. These bacteria, fungi, viruses, and archaea interact with their host in ways that extend far beyond digestion. The paper explores how these organisms communicate bidirectionally with the brain through what scientists call the brain-gut-microbiome (BGM) axis. This system shapes mood, cognition, and overall health from birth to old age.
Understanding the Brain-Gut-Microbiome Axis
The BGM axis links the gastrointestinal system to the central nervous system through multiple communication routes. These include the vagus nerve, immune signaling, microbial metabolites, neurotransmitters, and hormones. The gut microbiome produces vital molecules such as short-chain fatty acids, serotonin, dopamine, and gamma-aminobutyric acid. These compounds influence neural function and behavior.
When the microbiome maintains a balanced composition—known as eubiosis—it supports stable immune and metabolic activity. However, disruption of this balance, called dysbiosis, triggers inflammation, compromises gut barriers, and may alter brain chemistry. Stress, diet, and antibiotics can all initiate dysbiosis, leading to cognitive or emotional disorders such as depression and anxiety.
Immune and Inflammatory Interactions
The gut maintains a constant dialogue with the immune system. A healthy microbiome provokes a resting inflammatory state, where immune cells release protective cytokines without overreacting. When dysbiosis occurs, harmful bacteria can cross weakened gut barriers, enter circulation, and provoke systemic inflammation. This process affects the hypothalamic-pituitary-adrenal axis and contributes to neuroinflammatory conditions including Alzheimer’s and schizophrenia.
The epithelial layer and mucus barrier form the first lines of defense against invading microbes. Stress and toxins can damage these structures, allowing bacterial fragments such as lipopolysaccharides to activate immune responses. Continuous exposure to such fragments amplifies inflammation and links gut imbalance to brain dysfunction.
Chemical Communication Through Neurotransmitters
Microbial species synthesize and modulate neurotransmitters essential for brain function. Lactobacillus and Bifidobacterium produce gamma-aminobutyric acid, which regulates anxiety. Escherichia and Enterococcus can generate serotonin precursors from tryptophan metabolism. Changes in these bacterial populations influence mood and stress resilience. Reduced short-chain fatty acid production also impairs microglial activity, disrupting cognitive health. These discoveries suggest that microbes directly shape the brain’s chemical environment.
Microbiome Development from Birth
Early microbial exposure sets the stage for lifelong health. Once considered sterile, the intrauterine environment may already expose the fetus to microbial DNA and metabolites. These maternal signals might prime the newborn’s immune system before birth.
After birth, delivery method strongly affects microbial colonization. Infants born vaginally acquire beneficial bacteria such as Bacteroides and Lactobacillus, while those delivered by Cesarean section harbor more skin-associated microbes like Staphylococcus. A recent clinical study revealed that transferring maternal vaginal microbiota to Cesarean-born infants improved neurodevelopment within six months.
This evidence shows how early microbial exposure shapes both gut and brain development.
Microbes Through Life Stages
The gut ecosystem evolves continuously. During childhood, diet, antibiotics, and environmental factors shift microbial diversity. In adulthood, stable microbial communities maintain immune balance and energy metabolism. Aging brings a decline in beneficial bacteria and short-chain fatty acid production, contributing to inflammation and chronic disease.
Elderly individuals often show reduced Firmicutes and Bifidobacterium species, alongside increases in pathogenic Bacteroidetes. These shifts are associated with cognitive decline, mild cognitive impairment, and neurodegenerative diseases like Alzheimer’s and Parkinson’s.
Microbial Links to Neurodevelopmental Disorders
The paper highlights compelling connections between the microbiome and childhood brain disorders. Children with autism spectrum disorder often have fewer Firmicutes and more Bacteroidetes. They also show elevated Clostridium species, which release neuroactive metabolites that affect behavior.
Therapeutic interventions like fecal microbiota transplantation have shown promising results. In one study, children who received this treatment displayed lasting improvements in social interaction and gut health even two years later. However, larger randomized trials are needed to confirm its safety and effectiveness.
Dysbiosis and Adult Mental Health
Microbial imbalance affects neurotransmitter synthesis and the body’s stress response. Decreased short-chain fatty acid levels and increased inflammatory signaling have been linked to depression and anxiety. Certain Lactobacillus strains alleviate stress behaviors in animal models, while a disrupted vagus nerve eliminates these effects. This shows the importance of neural communication in translating gut signals to emotional outcomes.
Chronic inflammation driven by dysbiosis can also heighten the risk of neurodegenerative diseases. For instance, Parkinson’s disease correlates with increased Ruminococcaceae and decreased Prevotellaceae, leading to altered fatty acid metabolism and dopaminergic dysfunction.
Microbial Role in Stroke and Systemic Diseases
Gut imbalance influences cardiovascular and neurological outcomes. Stroke patients often exhibit fewer short-chain fatty acid-producing bacteria such as Faecalibacterium and Roseburia, with a rise in inflammatory microbes like Enterococcus. This pattern promotes atherosclerosis and worsens recovery outcomes.
Such findings highlight that gut health not only affects the brain directly but also shapes vascular health through immune and metabolic pathways.
Restoring Balance: Diet and Gut Biotics
A key section of the paper focuses on strategies to manage dysbiosis. Dietary modification remains the most natural and accessible method. High-fiber foods, fermented products, and prebiotic fibers encourage beneficial bacterial growth. Pregnant women who consumed fermented foods like yogurt and miso had children with improved early neurodevelopment.
The term “gut biotics,” introduced by Alagiakrishnan and Halverson, covers a broad range of interventions—including probiotics, prebiotics, postbiotics, and synbiotics—that restore gut balance. Probiotics like Lactobacillus and Bifidobacterium improve metabolism and immunity, while postbiotics (dead bacterial components) prevent pathogen adhesion on intestinal walls.
Prebiotics, Synbiotics, and Mental Well-Being
Prebiotics serve as food for good microbes, promoting the production of short-chain fatty acids and beneficial metabolites. Combining probiotics and prebiotics into synbiotics enhances these effects. In clinical studies, prebiotics have reduced obesity risk, improved glucose metabolism, and lessened allergic conditions in children.
Synbiotic supplementation alongside antidepressants also improved mood in patients with moderate depression compared to drug therapy alone. This finding reinforces that targeting the gut can complement psychiatric treatment.
Fecal Microbiota Transplantation: The Frontier Therapy
Fecal microbiota transplantation introduces healthy donor microbiota into a patient’s gut to restore microbial balance. It has shown positive outcomes for obesity, metabolic diseases, and even Alzheimer’s symptoms. While these results are promising, standard guidelines and safety protocols are still under development.
The Path Forward
The paper concludes that maintaining a healthy microbiome throughout life can prevent chronic inflammation and promote neurological resilience. Nutritional modulation, gut biotics, and microbiome-targeted therapies may act as synergistic treatments with conventional medicine.
Future research should focus on randomized clinical trials, standardized protocols for microbiota modulation, and understanding personalized microbial signatures. The gut’s microbial community may one day become a cornerstone of holistic healthcare—bridging mental and physical well-being through the smallest forms of life inside us.
The study is published in the Journal of Integrative Neuroscience. It was led by researchers from University of Toronto.