Ageing is an inevitable process marked by the gradual decline of physiological function and increased vulnerability to diseases. While the concept of ageing may often conjure images of gray hair or wrinkles, the molecular processes underlying this phenomenon are far more intricate. Among these, cellular senescence has emerged as a critical hallmark of ageing, influencing tissue function and organ health.
Recent research by Park et al., published in Experimental & Molecular Medicine, sheds light on the distribution and impact of p16INK4A+ senescent cells in elderly tissues, with a particular focus on immune cell senescence and epithelial dysfunction.
Cellular Senescence: A Double-Edged Sword
Cellular senescence refers to a state where cells irreversibly cease to divide. This process can be triggered by various stressors, including DNA damage, oxidative stress, and telomere shortening.
Senescent cells secrete inflammatory molecules, growth factors, and proteases—collectively termed the senescence-associated secretory phenotype (SASP). While SASP plays beneficial roles in processes like wound healing and tumor suppression, its chronic presence can drive tissue dysfunction and age-related diseases.
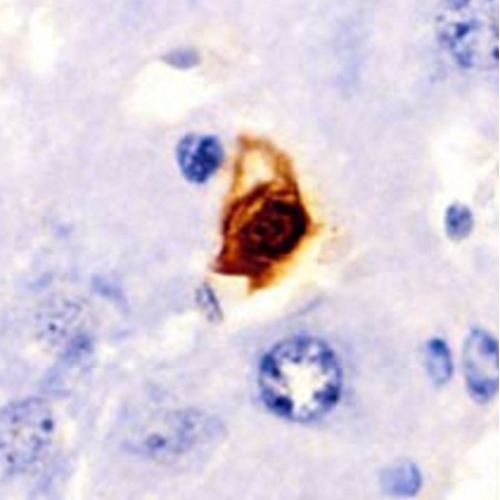
Park et al.’s study highlights p16INK4A, a widely recognised marker of cellular senescence, to investigate how senescent cells accumulate and influence tissues during ageing. Their findings emphasise the unique distribution of p16INK4A+ cells, revealing critical insights into organ ageing and immune cell dysfunction.
Mapping Senescent Cells in Tissues
The study introduces a “Senescence Atlas” to identify the distribution of senescent cells in the parenchyma and stroma of various tissues, including the colon, liver, skin, and lungs.
The authors found that fully senescent p16INK4A+ cells were surprisingly scarce in both the parenchyma—composed of functional cells—and the structural stromal cells, such as fibroblasts and smooth muscle cells. Instead, the majority of senescent cells were localised within immune cell populations, particularly T cells.
This observation challenges the traditional assumption that parenchymal cells primarily drive tissue ageing. Instead, immune cells, especially senescent T cells, emerged as key players in disrupting tissue homeostasis. These findings suggest a paradigm shift in understanding the mechanisms of ageing at the cellular level.
Impact of Senescent T Cells on Epithelial Integrity
Among the most striking findings of the study was the role of senescent T cells in compromising epithelial function.
Using advanced techniques like single-cell RNA sequencing (scRNA-seq) and immunohistochemistry, the researchers demonstrated that p16INK4A+ senescent T cells induce apoptosis and inflammation in colonic epithelial cells through the Granzyme A (GzmA)-protease-activated receptor (PAR) signaling pathway. This pathway led to the activation of inflammatory and apoptotic signals, impairing epithelial integrity and function.
The GzmA-PAR Axis
Granzyme A, a serine protease secreted by senescent T cells, activates PAR1 and PAR2 receptors in colonic epithelial cells. Activation of PAR1 triggers apoptotic pathways, while PAR2 activation leads to chronic inflammation. Together, these effects compromise epithelial cell viability and contribute to the functional decline observed in aged tissues.
Validation Through In Vitro Models
The researchers developed a senescent T cell model to validate these findings. By isolating and stimulating T cells from peripheral blood, they induced senescence and examined the effects of these cells on colonic epithelial cells. The results were consistent with in vivo observations: senescent T cells increased caspase-3/7 activity (a marker of apoptosis) and inflammatory cytokine expression in epithelial cells. Importantly, inhibiting GzmA reduced these detrimental effects, highlighting its potential as a therapeutic target.
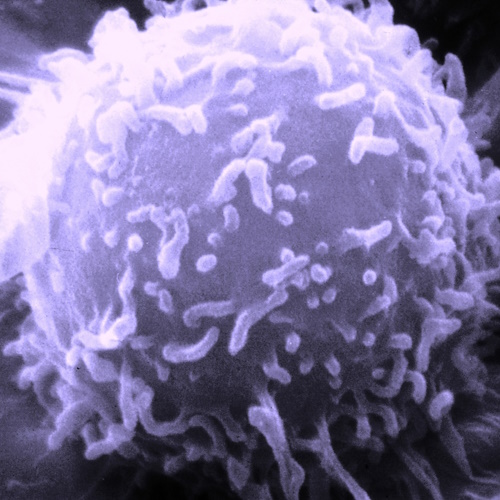
Immunosenescence: A Driver of Ageing
The study’s findings align with the concept of immunosenescence, which refers to the ageing-associated decline in immune system function. Immunosenescence is characterised by the accumulation of dysfunctional immune cells, chronic low-grade inflammation (often termed “inflammaging”), and impaired tissue repair.
Hallmarks of Senescent T Cells
Park et al. observed several hallmarks of senescent T cells, including increased expression of p16INK4A, reduced proliferation capacity, and elevated production of inflammatory molecules like GzmA. These cells exhibited “bystander activation,” meaning they could be activated independently of antigens. This property allows them to influence their microenvironment even in the absence of traditional immune triggers, further exacerbating tissue dysfunction.
Distribution Across Tissues
While senescent immune cells were identified across multiple tissues, their impact varied depending on the organ. For example:
- Colon: Senescent T cells interacted with epithelial cells, inducing apoptosis and inflammation.
- Skin: Senescence was more prominent in T cells than in fibroblasts or keratinocytes.
- Liver: Kupffer cells, the liver’s resident macrophages, showed significant signs of senescence.
These organ-specific variations underscore the complexity of immune cell senescence and its diverse effects on tissue ageing.
Implications for Anti-Ageing Therapies
The findings from Park et al.’s study have profound implications for developing anti-ageing interventions. By targeting senescent immune cells, particularly T cells, it may be possible to alleviate age-related tissue dysfunction and improve overall health in elderly individuals.
Senolytics and Senomorphics
Therapies aimed at removing senescent cells (senolytics) or modulating their secretory profile (senomorphics) have shown promise in preclinical studies. For instance, drugs that inhibit GzmA could potentially mitigate the detrimental effects of senescent T cells on epithelial tissues. Similarly, PAR antagonists could disrupt the inflammatory and apoptotic pathways activated by senescent cells.
Immunomodulation
Restoring immune system function is another promising strategy. Enhancing the clearance of senescent cells by immune cells or rejuvenating the thymus to improve T cell production could help counteract immunosenescence.
Personalised Medicine
The study’s Senescence Atlas provides a valuable resource for identifying tissue-specific patterns of senescence. This information could guide personalised interventions tailored to the unique ageing profiles of different organs.
Unanswered Questions and Future Directions
While the study provides critical insights, several questions remain unanswered:
What drives immune cell senescence?
The specific triggers and mechanisms underlying T cell senescence need further investigation. Factors like thymic involution and chronic antigenic stimulation are likely contributors.
How do other cell types contribute?
While this study focused on immune cells, the role of intermediate-stage senescent cells, such as fibroblasts, warrants further exploration.
Can senescent cells be repurposed?
Emerging evidence suggests that senescent cells may play beneficial roles under certain conditions. Understanding these dual roles could inform more nuanced therapeutic approaches.
What are the systemic effects?
Senescent cells secrete SASP factors that can influence distant tissues. The systemic impact of senescent T cells on ageing and disease progression remains to be elucidated.
Redefining Ageing
The study by Park et al. underscores the pivotal role of senescent immune cells in driving tissue dysfunction during ageing. By highlighting the unique distribution and effects of p16INK4A+ cells, it challenges traditional views of ageing and opens new avenues for therapeutic interventions.
Targeting senescent T cells and their downstream signaling pathways offers a promising strategy for mitigating the effects of ageing. As research continues to unravel the complexities of cellular senescence, we move closer to understanding and potentially reversing the mechanisms underlying age-related decline. Ageing may be inevitable, but its impact on our health and quality of life is increasingly within our control.
The study is published in the journal Experimental & Molecular Medicine. It was led by Soon Sang Park and team from Ajou University Medical Center, Suwon, Korea.