Key points from article :
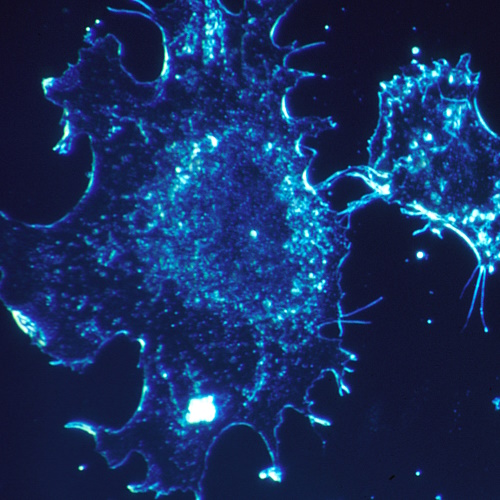
Research from the University of California, Los Angeles, found that conventional imaging may not reliably detect metastases in prostate cancer patients. The study examined 182 individuals previously classified as non-metastatic based on standard imaging. By using PSMA-PET/CT, a more advanced imaging technique, researchers discovered that 46% of these patients actually had metastatic cancer, with 24% showing five or more metastases. PSMA-PET works by using small amounts of radiotracers to bind to prostate cancer cells, making them visible during PET imaging, and has gained traction in the U.S. since the first radiotracer approval three years ago.
The study, led by Adrien Holzgreve at UCLA’s David Geffen School of Medicine, underscores the critical role of PSMA-PET in accurately staging prostate cancer. Calais emphasized its potential to significantly influence treatment decisions and outcomes. The research was published in JAMA Network Open and involved patients eligible for the EMBARK Phase III trial, which tested therapies for high-risk prostate cancer. Eligibility for this trial required conventional imaging to rule out metastases, yet PSMA-PET revealed previously undetected metastatic disease in nearly half the participants.
Holzgreve noted that while they expected PSMA-PET to detect more metastases than conventional imaging, the high number of findings in a carefully selected patient group was striking. The study supports the growing evidence that PSMA-PET is superior in providing accurate diagnostic and prognostic information compared to traditional methods. However, Holzgreve added that more high-quality prospective data is needed to confirm its superiority for guiding treatment decisions.
Despite being relatively new, PSMA-PET is increasingly recognized as a powerful tool in prostate cancer care, allowing more personalized therapies and improved staging accuracy. The researchers are optimistic about its continued role in advancing the understanding and treatment of prostate cancer.



/psma-pet-imaging-improves-prostate-cancer-metastases-detection.jpg)


