For centuries, physicians saw the gut as a simple digestive machine, a tube that breaks down food and absorbs nutrients. Only in the past two decades has science uncovered a richer truth. Our intestines host trillions of microorganisms, a hidden society working in constant dialogue with the human body. These organisms, collectively known as the gut microbiota, shape immunity, metabolism, and even mood. Today, evidence is mounting that they may also shape the fate of the heart.
Heart failure remains one of the deadliest outcomes of cardiovascular disease. Despite modern advances, survival rates have improved only modestly. Researchers now suspect that changes in gut microbes could accelerate or slow the course of this illness. The gut and the heart, once studied separately, are now understood as partners in health and disease.
Shifting landscapes in the gut
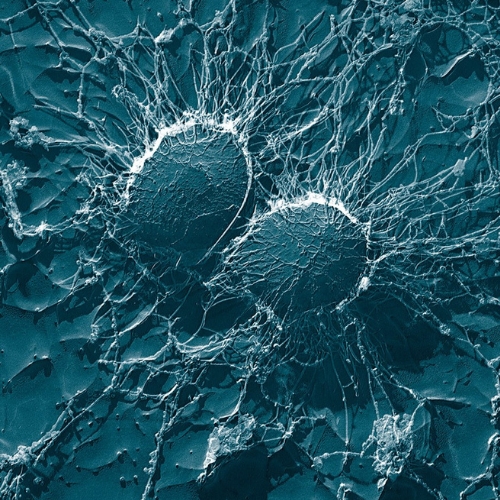
When the heart weakens, its pumping power drops. This reduced flow starves the intestines of blood, damaging the barrier that normally protects the body from invading toxins. At the same time, the microbial ecosystem shifts. Beneficial groups like Lactobacillus and Bifidobacterium decline, while more harmful species expand. This imbalance, often called dysbiosis, creates a leaky environment. Microbial fragments and metabolites slip through the weakened barrier into circulation, where they fuel inflammation and injury.
The pattern is not random. In patients with heart failure, scientists often find more Proteobacteria and Candida, groups linked with infection and inflammation. Meanwhile, bacteria that produce helpful short-chain fatty acids become scarce. This suggests that the failing heart and the failing gut form a feedback loop, each worsening the other.
Messages written in molecules
Microbes communicate with the body through the compounds they release. One of the most studied is trimethylamine N-oxide, or TMAO. Produced when bacteria digest nutrients like choline from eggs or red meat, TMAO acts as a pro-inflammatory signal. Elevated levels of TMAO stiffen arteries, heighten clotting risk, and promote fibrosis in the heart muscle. Patients with higher TMAO levels consistently face worse outcomes, and animal studies confirm its damaging potential.
Not all messages are harmful. Short-chain fatty acids, created when microbes ferment dietary fiber, play a protective role. They nourish intestinal cells, fortify the barrier, and reduce systemic inflammation. They even provide the heart with an alternative energy source when fatty acid metabolism falters. In this way, diet and microbial balance shape whether the molecular conversation leans toward healing or harm.
Bile acids and amino acids
Other compounds also carry weight in this dialogue. Bile acids, originally produced by the liver, are chemically reshaped by gut microbes. In healthy states, these acids help digest fats. But in heart failure, their balance shifts toward more toxic forms that promote cellular stress and chronic inflammation. Some research links these shifts with poorer survival in patients.
Amino acid byproducts tell a similarly complex story. Certain derivatives worsen heart function by disrupting energy metabolism, while others provide alternative fuel that supports cardiac cells. In some experimental models, replacing specific amino acids or transplanting healthy microbiota restores balance and protects against decline. These findings show that the molecular web connecting gut and heart is intricate, with both harmful and helpful strands.
Immune ties between gut and heart
Beyond metabolism, immunity forms another bridge. A balanced microbiota helps train immune cells, keeping inflammation under control. Dysbiosis, by contrast, sparks low-grade inflammation that damages tissues throughout the body, including the heart. Excessive activation of immune pathways can drive fibrosis, hypertrophy, and progressive loss of function.
Animal models highlight this vividly. When healthy microbes are restored—through probiotics, high-fiber diets, or even fecal transplants—hearts recover more effectively after injury. In some cases, transplanting microbiota from healthy donors reduces inflammation and improves cardiac performance. These studies reveal that the immune system listens closely to the microbial orchestra, with consequences that extend far beyond the intestines.
Exploring therapies through microbes
Armed with this knowledge, researchers are testing new ways to reshape the gut ecosystem. Probiotics show early promise by boosting beneficial strains and shifting metabolic outputs toward protective short-chain fatty acids. Dietary changes, particularly those rich in fiber or modeled on Mediterranean traditions, improve microbial diversity and reduce markers of inflammation. Some clinical trials even suggest benefits for heart patients who adopt these patterns.
Fecal microbiota transplantation, though still experimental in this field, has already proven safe and effective for intestinal infections. In animal models of heart disease, it improves cardiac structure and function. Antibiotics, on the other hand, carry more risk. While they can reduce harmful bacteria temporarily, they may also wipe out protective strains, sometimes worsening outcomes. This duality highlights the need for caution.
Looking toward the future
The interplay between gut microbes and heart failure remains a young science. Many questions are open. Do microbial shifts cause heart failure, or do they simply accompany it? Which metabolites hold the most sway, and how can they be targeted safely? Can therapies be tailored to each patient’s unique microbial signature?
What is clear is that the gut and heart are not strangers. They share a two-way conversation that shapes health across a lifetime. By understanding this dialogue, medicine may uncover new paths to protect the heart—not only with drugs and devices, but also with diet, microbes, and lifestyle choices. The next chapter of cardiovascular medicine may be written not in the arteries, but in the intestines.
The study is published in the journal Genes & Diseases. It was led by researchers from Wuhan University.