Modern medicine has pushed the boundaries of human health, but the challenge of slowing biological ageing remains. While we have treatments for specific diseases, few therapies directly address the cellular changes that accompany growing older. One of the most important biological drivers of ageing is cellular senescence—a process in which damaged cells stop dividing but do not die. These senescent cells accumulate in organs, releasing harmful molecules that promote inflammation, tissue damage and chronic disease.
Now, researchers are exploring whether an existing class of anti-diabetic medications—SGLT2 inhibitors—could be repurposed to target senescent cells. These drugs, originally developed to lower blood sugar in people with type 2 diabetes, appear to also act on several ageing-related pathways. They may reduce inflammation, restore mitochondrial health, and even extend lifespan in animal studies. Could a simple pill designed for diabetes also delay the ageing process?
Understanding the Mechanism of Senescence
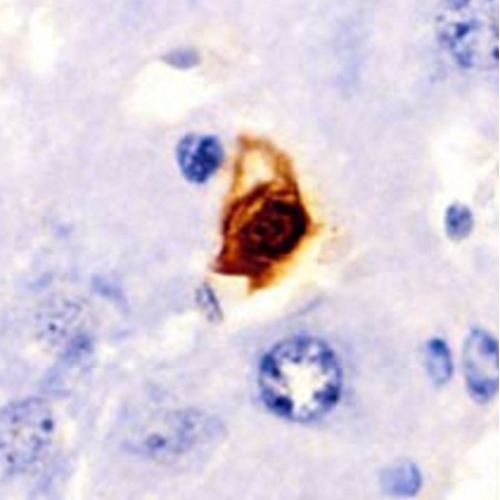
Cellular senescence was first described in the 1960s when scientists noticed that human fibroblasts eventually stopped dividing in culture. This irreversible arrest, triggered by DNA damage or telomere shortening, is now known to contribute to tissue dysfunction. Senescent cells resist apoptosis and release a toxic cocktail of cytokines and enzymes known as the senescence-associated secretory phenotype, or SASP.
The SASP affects nearby cells and creates a low-grade, chronic inflammatory state. Over time, this drives the development of conditions such as heart disease, type 2 diabetes, neurodegeneration, and cancer. Eliminating or suppressing senescent cells is now considered a cornerstone of anti-ageing therapy.
From Glucose Control to Cellular Rejuvenation
SGLT2 inhibitors such as dapagliflozin, canagliflozin, and empagliflozin were originally introduced to treat type 2 diabetes by promoting glucose excretion through the kidneys. They act on the sodium-glucose co-transporter 2 in renal tubules, lowering blood sugar without affecting insulin levels. What surprised researchers was the discovery that these drugs also protect the heart and kidneys, and reduce hospitalisation and mortality—even in patients without diabetes.
Clinical trials such as EMPA-REG, CANVAS and DECLARE-TIMI 58 showed fewer cardiovascular events in patients treated with SGLT2 inhibitors. These effects occurred independently of glucose control, prompting scientists to investigate their underlying biology. Attention soon turned to their impact on senescent cells.
Diabetes and Senescence: A Vicious Loop
Type 2 diabetes accelerates cellular senescence. High blood sugar generates reactive oxygen species, damages DNA, and promotes the release of inflammatory molecules. In return, senescent cells in the pancreas and immune system worsen metabolic dysfunction. This cycle contributes to the progression of diabetes and its complications.
In lab studies, endothelial cells and cardiomyocytes exposed to high glucose showed elevated markers of senescence, including SA-β-gal activity, p21, and p16 expression. Treatment with SGLT2 inhibitors significantly reduced these markers. In essence, the drugs appear to interrupt the feedback loop between hyperglycaemia and senescence.
Targeting Blood Vessels: Fighting Endothelial Ageing
Endothelial cells, which line blood vessels, are particularly vulnerable to senescence. Their dysfunction leads to reduced nitric oxide production, poor vasodilation, and increased cardiovascular risk. In ageing and diabetes, senescent endothelial cells accumulate and amplify damage to the vascular system.
SGLT2 inhibitors improve endothelial function by reducing oxidative stress, increasing nitric oxide, and activating protective proteins like SIRT1 and AMPK. For example, in high-glucose models, dapagliflozin restored nitric oxide production and reversed senescence in human umbilical vein endothelial cells. Similar effects were observed with empagliflozin and canagliflozin.
Interestingly, toxins like nanoplastics and certain cancer drugs induce endothelial senescence by increasing SGLT2 expression. Blocking SGLT2 reversed this damage. This suggests that vascular protection is not just a secondary benefit—it may be central to how these drugs work.
Cardiovascular Protection Through Mitochondrial Repair
The heart is highly susceptible to the damage caused by senescent cells. Ageing impairs cardiac function, increases fibrosis, and promotes inflammation. In diabetic animal models, SGLT2 inhibitors improved heart health by restoring mitochondrial dynamics and reducing oxidative stress.
Empagliflozin was found to suppress mitochondrial fission and reduce fibrosis in heart failure models. It also modulated key ageing pathways such as AMPK and SIRT1. In one study, empagliflozin protected against doxorubicin-induced cardiotoxicity, a common side effect of chemotherapy, by preserving the STAT3 pathway.
Even more compelling is the observation that SGLT2 inhibitors improve calcium signalling in ageing cardiomyocytes. They appear to restore normal mitochondrial function, reduce apoptosis, and support cardiac regeneration.
Kidney Ageing and Diabetic Nephropathy
Age-related decline in kidney function is accelerated by diabetes. Senescent tubular cells in the kidney release SASP factors that trigger fibrosis and chronic inflammation. Studies show that high glucose increases SGLT2 expression in renal cells, along with DNA damage and oxidative stress.
Dapagliflozin and canagliflozin reduce these effects by lowering ROS levels and suppressing senescence markers. In one model, SGLT2 inhibition improved kidney ageing in non-diabetic mice, surpassing the effects of metformin. This suggests that SGLT2 inhibitors may act directly on renal ageing pathways, offering protection even in the absence of diabetes.
Regeneration and Stem Cell Preservation
Stem and progenitor cells decline with age, leading to reduced tissue repair and regeneration. In studies of human bone marrow mesenchymal stem cells, empagliflozin enhanced proliferation and reduced senescence. It also improved the therapeutic potential of stem cells in heart repair after injury.
Moreover, in diabetic patients, empagliflozin increased circulating progenitor cells with vascular regenerative capacity. This indicates that SGLT2 inhibitors may restore not just damaged cells but also the systems needed to replace them.
Adipose, Liver and Brain Benefits
In obese and diabetic animals, SGLT2 inhibitors reduced senescence in adipose tissue and liver. They lowered inflammatory signals like IL-6 and TNF-α, and reduced fibrosis. In naturally aged mice, empagliflozin downregulated key senescence markers and improved liver health.
Cognitive function also improved in aged mice treated with dapagliflozin. The treatment boosted antioxidant defences and upregulated SIRT1 in brain tissue. These results suggest that SGLT2 inhibitors may provide neuroprotection and counter age-related cognitive decline.
Extending Lifespan: Evidence from Animal Studies
Perhaps the most striking findings come from lifespan studies. In mouse models, treatment with canagliflozin or empagliflozin extended lifespan and improved healthspan. The drugs mimicked the effects of calorie restriction by modulating nutrient-sensing pathways like AMPK, mTOR, and SIRT1.
Interestingly, these benefits were more consistent in male mice. Female mice did not show the same lifespan extension, raising important questions about sex-specific responses. Future trials must include both sexes to confirm these findings in humans.
A Call for Human Trials and Deep Phenotyping
Despite promising animal data, human trials are essential to validate these effects. The TAME trial, which is testing metformin in non-diabetic older adults, serves as a useful model. A similar trial could test SGLT2 inhibitors for their anti-ageing effects in healthy or pre-frail individuals.
Future studies should use deep phenotyping, including biomarkers from blood, urine, and tissue. Technologies like digital twins and multi-omics analysis could predict how SGLT2 inhibitors affect organs, systems, and senescence patterns in real time.
Conclusion: Bridging Metabolism and Longevity
The repurposing of SGLT2 inhibitors marks a promising frontier in geroscience. These drugs do more than control diabetes—they act on core ageing mechanisms. By reducing senescence, restoring mitochondrial function, and improving regenerative capacity, they offer a new strategy for age-related diseases.
Their broad effects on the heart, kidneys, liver, brain, and blood vessels make them ideal candidates for multi-targeted interventions. While more research is needed, especially in human populations, SGLT2 inhibitors may soon join the toolkit of therapies designed not just to treat—but to delay—ageing itself.
The study is published in the journal Npj Aging. It was led by Georgina M. Ellison-Hughes from King’s College London.