Key points from article :
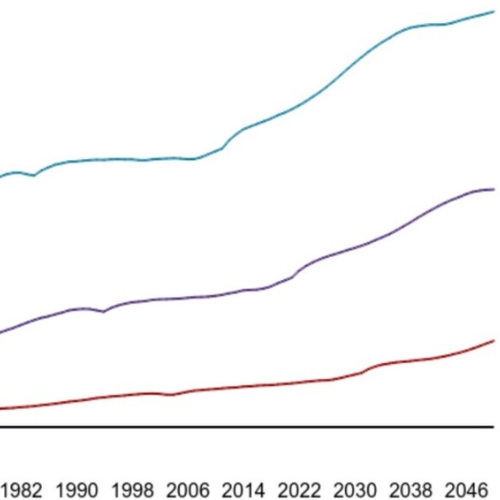
A major new analysis led by David Leon and colleagues at the London School of Hygiene and Tropical Medicine, published via medRxiv and the LSHTM website, highlights troubling trends in the UK's mortality rates compared to other high-income nations. Commissioned by the Health Foundation, the study shows that since the 2010s, improvements in UK mortality have slowed significantly—more than in most peer countries. By 2023, UK mortality rates were 14% higher for women and 9% higher for men compared to the median of 21 other wealthy nations.
The research reveals sharp geographic and age-related inequalities. Scotland, Wales, and Northern Ireland all have higher mortality rates than England, with Scotland performing particularly poorly. Mortality is especially concerning among people aged 25–49: UK women in this age group had a mortality rate 46% higher than the international median in 2023, and for men it was 31% higher. Deaths from external causes—such as injuries and drug-related deaths—are driving this trend, explaining up to 80% of the divergence with peer countries.
The UK’s rising rate of drug-related deaths is a key concern. These deaths tripled between 2001 and 2019, diverging sharply from the decline seen in other nations. The impact is particularly stark in Scotland and northern England, where drug-related mortality is up to four times higher than in London. The authors argue that these trends are rooted in socioeconomic deprivation and a failure to invest in public health and prevention services.
The briefing concludes that without bold, long-term action—including tackling poverty, boosting regional economies, resourcing local public health services, and addressing drug misuse—the UK risks falling further behind its international peers. A cross-government strategy focused on reducing health inequalities and improving working-age health is urgently needed.