Can Magnetic Fields Mimic Exercise? A New Study Explores a Novel Therapy for Type 2 Diabetes
A Fresh Approach to an Old Problem
Type 2 diabetes mellitus (T2DM) is one of the fastest-growing chronic diseases in the world, tightly linked to insulin resistance, excess visceral fat, and mitochondrial dysfunction. Doctors consistently recommend lifestyle changes—especially regular endurance exercise—to help patients lower blood sugar and reduce long-term health risks. But meeting the guidelines isn’t easy. Many people with T2DM are older, experience joint pain, or have limited mobility, making sustained exercise difficult.
What if some of the metabolic benefits of exercise could be triggered without physical exertion?
A team of researchers led by Fan Shuen Tseng and colleagues, reporting in the Journal of Clinical Medicine (2025), investigated a novel technology called magnetic mitohormesis (MM). This treatment uses very low-dose pulsed electromagnetic fields (PEMF) to gently stimulate skeletal muscle mitochondria—the same cellular pathways activated by endurance exercise.
Early laboratory and animal studies suggest PEMF can enhance mitochondrial respiration, improve fatty-acid metabolism, and reduce markers of inflammation. But until now, no clinical study had directly tested whether MM could improve blood-sugar control in people living with T2DM.
What Is Magnetic Mitohormesis?
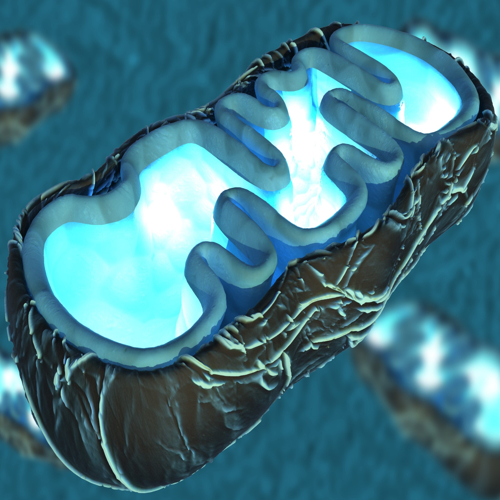
Mitohormesis refers to the idea that mild stress applied to mitochondria—the “power plants” of cells—can strengthen them over time. Exercise is a classic example: muscle fibers experience temporary stress, triggering repair pathways that enhance mitochondrial efficiency and energy production.
MM seeks to replicate this effect using short, weekly exposures to magnetic fields. The fields are weak enough to be safe and comfortable, but strong enough to activate calcium-dependent mitochondrial signaling pathways that drive adaptations similar to aerobic training.
Think of it as a biological “nudge” to the muscle’s metabolic machinery.
Inside the Study: Who Participated and What Happened?
The research team conducted an exploratory clinical study involving 40 adults aged 40–75 with suboptimally controlled T2DM (HbA1c between 7.0% and 10.0%). Most participants had lived with diabetes for more than a decade and were already taking standard glucose-lowering medications. Importantly:
- 97.5% were physically inactive or minimally active.
- 70% had obesity, and 22.5% had central obesity, defined as a waist-to-hip ratio (WHR) ≥ 1.0.
- No participants changed their diet or medication during the study.
The Treatment
Each person received 12 weekly MM sessions. During each 10-minute session, participants placed one leg inside a chamber that delivered low-frequency PEMF; the opposite leg was treated the following week. This alternating-leg schedule continued for three months.
Researchers measured metabolic markers—including fasting glucose, insulin resistance (HOMA-IR), and HbA1c—before and after treatment.
What Did the Scientists Find?
On the surface, the overall results were modest. Among all 40 participants, MM treatment did not significantly change:
- HbA1c
- Fasting glucose
- Fasting insulin
- Insulin resistance
- Body weight or body composition
However, a striking pattern emerged when researchers dug deeper.
Benefits for People with Central Obesity
Participants with central obesity—those carrying the highest levels of visceral fat—responded very differently.
- 88.9% of centrally obese patients showed a reduction in HbA1c after treatment.
- In comparison, only 32.3% of participants without central obesity improved.
- Their median HbA1c dropped from 7.5% to 7.1%—a statistically significant improvement (p < 0.01).
This magnitude of reduction (about 0.4%) is comparable to the lower end of what aerobic exercise typically achieves in clinical trials.
Why the difference? Visceral fat is known to produce harmful metabolic byproducts, including ceramides, that worsen insulin resistance. Previous PEMF research showed reductions in visceral adiposity and ceramide levels, suggesting that people with high central fat may have more to gain from mitohormetic stimulation.
Why This Matters
The findings offer early but intriguing evidence that MM could serve as a complementary therapy for people with T2DM—especially for those unable to perform regular exercise.
Key Advantages
- Completely non-strenuous: No physical exertion required.
- Short sessions: Only 10 minutes a week.
- Excellent tolerability: 100% study retention, no adverse effects.
- Potential precision therapy: May benefit specific metabolic phenotypes, such as central obesity.
For clinicians treating older adults, or for patients facing mobility challenges, MM could someday fill a critical gap.
What’s Next for Magnetic Mitohormesis?
As a pilot study, this research has limitations: a small sample size, no control group, and a relatively short duration. The authors emphasize the need for large, randomized, double-blind trials to:
- Confirm the metabolic impact of MM
- Identify which patients benefit most
- Determine optimal treatment frequency and duration
- Explore combinations with modern diabetes medications (e.g., GLP-1 agonists, SGLT2 inhibitors)
Future studies may also incorporate metabolic phenotyping and lipidomic profiling to understand how MM alters inflammation, ceramide levels, and mitochondrial pathways.
The Bottom Line
Magnetic mitohormesis is an innovative, non-invasive approach that aims to harness the metabolic power of mitochondria—without breaking a sweat. While not a replacement for exercise, it may one day become a valuable tool for managing type 2 diabetes, particularly in individuals struggling with central obesity and limited mobility.
Early results are promising, and the next wave of clinical trials will reveal whether this technology can play a meaningful role in the future of metabolic health.
The study is published in the journal Journal of Clinical Medicine. It was led by Hong Chang Tan from Singapore General Hospital, Singapore.



/targeting-mitochondria-to-tackle-diabetes-inside-a-cutting-edge-clinical-trial.jpg)


