When we think about ageing, we imagine wrinkles, white hair, and slower movements. But while these changes are visible, the most dangerous effects of ageing happen quietly inside us — especially in our hearts and blood vessels. Over time, these organs lose flexibility and strength, making them vulnerable to heart attacks, heart failure, and strokes.
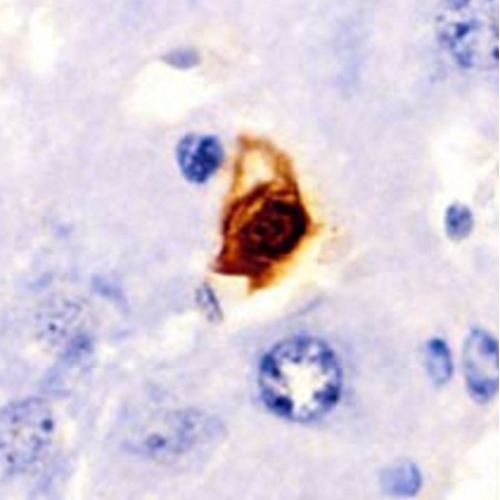
Scientists have long searched for ways to fight these hidden changes. One of the most fascinating new ideas is targeting senescent cells. These are cells that stop dividing but refuse to die. They act like "zombies" — stuck in place, releasing harmful molecules that damage nearby cells and speed up tissue ageing.
Could clearing these "zombie" cells rejuvenate our hearts? That’s the hope behind senolytic therapy. But while this approach shows promise, new research urges caution. Let's explore why.
Senescent cells: the secret troublemakers
As we age, cells face stress from DNA damage, oxidative stress, chronic inflammation, and even mechanical strain from blood flow. To avoid becoming cancerous, some cells enter a state called senescence. In this state, they stop dividing permanently but remain alive.
Instead of disappearing, senescent cells release a cocktail of harmful molecules known as SASP (senescence-associated secretory phenotype). These molecules include inflammatory signals, enzymes that break down tissue, and other factors that disturb the local environment.
In the cardiovascular system, senescent cells build up in heart muscle cells (cardiomyocytes), blood vessel linings (endothelial cells), immune cells, and supporting fibroblasts. This build-up leads to chronic inflammation, tissue stiffness, scarring, and poor repair after injury.
Evidence from animal models: a reason for hope
The first major clue that senescent cells could be targeted came from mouse studies. When researchers genetically removed senescent cells in ageing mice, the animals lived longer and showed better organ function.
Further studies focused on the heart. In mouse models of heart attacks, removing senescent cells reduced scarring (fibrosis) and improved heart pumping function. Mice also had better exercise capacity and vascular health after treatment with senolytic drugs like dasatinib and quercetin or navitoclax.
These experiments suggested a bold possibility: what if we could clean out these harmful cells and give hearts a second chance to function better, even at an old age?
The first warning signs: not all senescent cells are bad
Excitement around senolytic therapy grew fast. But new data quickly added complexity. Researchers discovered that some senescent cells are not only harmless but helpful.
After a heart attack, certain senescent cells release signals that guide repair and control scar formation. Some help stabilise tissues, preventing excessive damage. In the arteries, senescent cells in plaques may make them more stable, reducing the risk of sudden rupture and heart attacks.
Animal studies showed that removing these "helpful" senescent cells too early or too aggressively led to worse outcomes. Hearts functioned more poorly, and arteries became more unstable.
The risk of senolytic drugs: not just about the heart
Senolytic drugs were originally developed as cancer treatments. They target proteins that help cells avoid death, forcing them to self-destruct. But this approach is not selective.
These drugs can also harm healthy cells, including important immune cells and blood-forming cells. Side effects like low platelet counts, increased bleeding risk, and immune suppression have been observed. In some mouse studies, senolytic therapy led to higher death rates, especially when used on advanced atherosclerosis (severe artery disease).
The case of atherosclerosis: a double-edged sword
In atherosclerosis, plaques build up inside arteries, threatening to block blood flow or rupture. Senescent cells accumulate in these plaques and seem to play a complicated role.
Some studies showed that eliminating senescent cells reduces plaque size and inflammation. But others found the opposite: removing these cells weakened the plaques, made them thinner, and increased the risk of rupture and sudden death.
One striking study found that treatment with ABT-263, a strong senolytic drug, reduced the protective smooth muscle layer of plaques by 90%, leading to more plaque instability and a 50% increase in mortality in mice.
This stark warning suggests we cannot treat all senescent cells as "bad guys" without understanding their specific roles.
The new strategy: senomorphics
Given these risks, researchers began developing senomorphics. Instead of killing senescent cells, senomorphics aim to suppress their harmful secretions (the SASP) while keeping the cells alive.
This approach could preserve beneficial functions, like guiding repair and maintaining tissue structure, while reducing damaging inflammation.
Examples include drugs targeting the mTOR pathway, SIRT1 activators, and certain metabolic regulators. These compounds have shown promise in reducing harmful signals without completely wiping out the cells.
Thinking beyond: can we reverse cell senescence?
Another exciting idea is senoreversion, turning senescent cells back into healthy, active cells. Studies using exosomal microRNAs in mice suggest this might be possible.
Instead of destroying or silencing these cells, we could teach them to behave normally again. This approach remains in very early stages but could one day revolutionise how we tackle organ ageing.
Timing and precision: the missing pieces
One major challenge is timing. In heart disesse, clearing senescent cells too early after a heart attack might disrupt repair. Too late, and harmful effects might already be irreversible.
Another problem is precision. Current senolytic drugs are not selective enough. They act on many cell types and cannot distinguish between "good" and "bad" senescent cells.
Future therapies might need to target specific senescent cell types, or even single cell subgroups within plaques or heart tissue. Researchers are working on ways to tag and track different senescent cells, but this work is complex and still developing.
Human trials: a careful path forward
While animal studies give important clues, translating these results to humans is difficult. The human heart is larger, more complex, and responds differently to injuries and drugs.
There are ongoing human trials testing senolytics for other conditions like osteoarthritis, chronic kidney disease, and Alzheimer's. But for heart disease, no large-scale human trials have been completed yet.
We need careful, long-term studies to understand safety, optimal dosing, and timing. Until then, widespread use of senolytic therapy in heart disease remains premature.
Senescence and the bigger picture of ageing
Beyond the heart, senescent cells play roles in other organs: skin, lungs, liver, and pancreas. In some cases, they help protect against cancer, support wound healing, or maintain certain functions in older tissues.
Completely removing these cells might disrupt these protective effects, leading to unintended consequences.
Researchers are now exploring combined strategies: modulating senescent cells when needed, boosting their beneficial effects, and only removing them in specific situations.
The promise and the caution
Senolytic therapy represents a revolutionary idea. Imagine a world where we could clear out harmful cells and rejuvenate ageing hearts, potentially extending healthy lifespan.
However, as new studies show, the reality is more complex. Not all senescent cells are enemies. Some are quiet protectors. Some help us heal.
Killing all of them, without understanding their roles, risks causing more harm than good. That is why scientists now urge caution and call for more research before these treatments move into regular clinical use for heart patients.
Conclusion: a promising, unfinished journey
Senolytics may one day transform cardiovascular medicine and help us manage heart ageing more effectively. But today, they remain tools for the future, not ready answers for the present.
We need precision, better understanding, and patience. Only then can we truly unlock their potential safely and wisely.
The study is published in the journal Biomolecules. It was led by Zhihong Yang from University of Fribourg.