Ageing reshapes the human heart through cellular and molecular changes that influence function and disease risk. Cellular senescence, a process where cells permanently stop dividing while remaining metabolically active, stands at the center of this transformation. This process plays a complex dual role. It protects against malignancy and aids tissue repair, yet its chronic accumulation contributes to cardiovascular degeneration. Understanding and targeting cellular senescence may transform approaches to cardiovascular ageing and disease management.
Nature and Mechanisms of Cellular Senescence
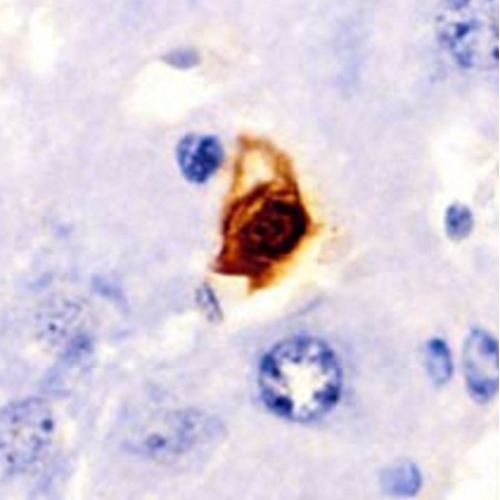
Cellular senescence represents an irreversible arrest of the cell cycle. It occurs when cells experience stressors such as DNA damage, oxidative stress, telomere shortening, or oncogenic activation. Unlike apoptosis, senescent cells remain metabolically active and secrete a range of pro-inflammatory factors known collectively as the senescence-associated secretory phenotype. These secreted molecules include cytokines, chemokines, growth factors, and proteases that influence surrounding cells and tissues.
In young organisms, transient senescence maintains tissue homeostasis and supports embryonic development, wound repair, and tumor suppression. However, persistent senescence becomes detrimental. Accumulated senescent cells disrupt the local environment, impair regeneration, and promote chronic inflammation, which underlies many age-related diseases including cardiovascular disorders.
Senescent cells display morphological changes such as enlarged cell size, altered nuclear architecture, and mitochondrial dysfunction. They also show metabolic reprogramming that favors glycolytic activity and reactive oxygen species production. These alterations collectively impair cellular function and accelerate tissue ageing.
Dual Roles of Senescence in the Cardiovascular System
Within the cardiovascular system, senescence serves both protective and harmful functions. During acute stress, senescent endothelial and stromal cells can promote healing by limiting cell proliferation and triggering immune clearance of damaged cells. Yet long-term persistence of senescent cells within blood vessels and cardiac tissue promotes fibrosis, vascular stiffness, and impaired contractility.
When the heart experiences injury or ischemia, senescent fibroblasts and cardiomyocytes accumulate and secrete inflammatory and fibrotic mediators. These signals alter communication among vascular, immune, and myocardial cells. Over time, this process leads to structural remodeling and reduced pump efficiency.
Studies show that eliminating senescent cells in animal models restores cardiac function, enhances ventricular remodeling, and improves survival. The removal of these cells also reduces systemic inflammation, emphasizing their causal role in cardiovascular ageing.
Senescence in Atherosclerosis
Atherosclerosis arises from endothelial dysfunction, lipid deposition, and chronic inflammation within arterial walls. Senescent endothelial and smooth muscle cells exacerbate these processes by losing their normal regulatory roles and adopting a pro-inflammatory phenotype.
Endothelial senescence impairs nitric oxide production, reducing vasodilation and promoting leukocyte adhesion. Smooth muscle cell senescence encourages abnormal collagen synthesis and plaque calcification. Together, these effects destabilize atherosclerotic plaques, making them prone to rupture and thrombosis.
Reducing senescent cell burden restores endothelial function and stabilizes plaques. Experimental findings suggest that controlled elimination of senescent cells or suppression of their secretory activity can slow plaque formation and enhance vascular resilience. These insights reveal cellular senescence as a central mechanism linking vascular ageing to atherosclerosis.
Senescence and Myocardial Infarction
Myocardial infarction triggers massive cardiomyocyte death due to oxygen deprivation. After such injury, senescent cells accumulate in cardiac tissue, where they impair healing and promote fibrosis. Senescent fibroblasts overproduce extracellular matrix proteins, leading to scar formation that stiffens the ventricular wall. Senescent cardiomyocytes, meanwhile, lose contractile capacity and secrete inflammatory molecules that damage nearby cells.
Targeting these senescent populations improves cardiac recovery. Removing senescent cells in preclinical models enhances angiogenesis, reduces scar size, and restores myocardial function. Activating pathways that counter senescence, such as those controlled by sirtuins, supports mitochondrial integrity and cell survival. Conversely, suppressing pro-senescence signals like p53 and p21 reduces maladaptive remodeling and preserves tissue elasticity.
Senescence and Heart Failure
Heart failure represents the terminal stage of many cardiovascular conditions. It is characterized by impaired pumping efficiency, structural remodeling, and chronic inflammation. Senescent cells accumulate in the myocardium and vascular endothelium, contributing to these pathologies.
With age, cardiomyocytes decline in number while the remaining cells enlarge and stiffen. Senescence of endothelial cells limits oxygen and nutrient delivery, worsening tissue hypoxia. Increased secretion of inflammatory mediators from senescent cells accelerates fibrosis and reduces myocardial compliance.
Restoring balance between cell renewal and senescence emerges as a therapeutic goal. Strategies that promote autophagy, enhance mitochondrial function, or remove senescent cells show promise in preclinical heart failure models. Yet the transition of these approaches to clinical practice requires deeper understanding of safety and timing.
Senescence in Cardiomyopathies and Arrhythmias
In genetic and acquired cardiomyopathies, premature senescence of cardiac cells drives disease progression. Shortened telomeres, mitochondrial dysfunction, and persistent DNA damage activate senescence pathways that weaken the myocardium.
Senescence in myocardial fibroblasts fosters fibrosis, while ageing cardiomyocytes disrupt electrical signaling and increase arrhythmogenic risk. Defects in nuclear envelope proteins can trigger senescence through DNA damage responses, linking structural mutations to chronic inflammation and contractile failure.
Targeting these pathways may alleviate fibrosis and improve cardiac rhythm stability. Understanding how senescence interacts with cellular stress in these disorders could yield precision treatments that slow or reverse disease evolution.
Metabolic and Epigenetic Influences
Metabolism and epigenetics profoundly shape cellular senescence. Disturbances in mitochondrial energy production and nicotinamide adenine dinucleotide balance drive oxidative stress and DNA damage. Lipid accumulation and hyperglycemia also accelerate senescence by altering energy-sensing pathways.
Specific enzymes involved in amino acid metabolism, such as those controlling serine biosynthesis, regulate senescence through effects on gene transcription. Disruption of these metabolic circuits enhances susceptibility to cardiovascular ageing.
Epigenetic regulation forms another critical layer. Modifications such as DNA methylation and histone acetylation alter gene expression patterns linked to ageing. Experimental evidence shows that restoring youthful epigenetic states can reverse physiological markers of ageing and improve organ function. These discoveries suggest that ageing stems largely from epigenetic drift rather than irreversible DNA mutations.
Therapeutic Strategies Targeting Senescence
Recent years have seen rapid advances in developing therapies that directly target senescent cells. Senolytics are compounds that selectively induce apoptosis in senescent cells while sparing healthy ones. By eliminating these dysfunctional cells, senolytics can rejuvenate tissues and extend lifespan in animal models.
Common senolytic combinations include small molecules that inhibit anti-apoptotic pathways active in senescent cells. These drugs improve vascular flexibility, reduce fibrosis, and restore organ performance. In cardiac ageing, senolytics enhance left ventricular function and reduce inflammatory signaling.
Beyond senolytics, senomorphics modulate the behavior of senescent cells without killing them. They suppress the secretion of harmful SASP factors, mitigating inflammation and tissue damage. Natural compounds such as resveratrol, spermidine, and rapamycin analogs belong to this category.
Sirtuins also represent key therapeutic targets. These NAD-dependent enzymes maintain genomic stability, regulate metabolism, and protect against oxidative damage. Enhancing sirtuin activity improves mitochondrial function and endothelial health, providing broad cardioprotective benefits.
Nutritional and Pharmacological Modulators
Nutrients influence the senescence network through antioxidant and anti-inflammatory effects. Vitamins, polyphenols, and metabolic cofactors reduce oxidative stress and stabilize DNA. For instance, folate supplementation lowers levels of cellular stress markers and improves cardiac structure in ageing models. Compounds that stimulate serine biosynthesis may further delay cardiovascular ageing by maintaining metabolic flexibility.
Other small molecules, including inhibitors of bromodomain proteins, modulate gene expression linked to senescence. Such interventions could correct transcriptional imbalances associated with chronic inflammation and tissue remodeling. Together, these findings suggest that targeting senescence is achievable through both pharmacological innovation and nutritional optimization.
Emerging Clinical Evidence
Several early-stage clinical studies now explore the safety and efficacy of anti-senescence strategies in cardiovascular disorders. Investigations involve compounds that either remove senescent cells or modulate their secretory activity. Preliminary results indicate improvements in vascular elasticity, reduced inflammation, and enhanced cardiac output.
However, translation from animal research to human therapy remains challenging. Differences in senescent cell types, tissue distribution, and drug sensitivity complicate dosing and risk assessment. Long-term studies are necessary to establish whether clearing senescent cells can sustain cardiovascular benefits without adverse effects.
Cellular Heterogeneity and Precision Medicine
Senescent cells are not uniform. They vary by tissue origin, gene expression profile, and response to stress. Recognizing this heterogeneity is essential for designing targeted therapies. Advanced computational and single-cell transcriptomic tools now classify senescent cells into distinct subtypes, each with unique molecular signatures.
Machine learning algorithms have enabled identification of senescent cell categories and prediction of their drug responses. These analytical frameworks reveal that some senescent subpopulations retain regenerative potential, while others drive chronic inflammation. Personalized therapy must therefore consider which senescent cells to eliminate and which to preserve.
Single-cell sequencing of aged cardiac tissue shows that specific fibroblast and immune cell clusters express genes linked to fibrosis, inflammation, and angiogenesis inhibition. Mapping these interactions clarifies how senescence propagates across cell types, guiding the development of precision anti-ageing interventions.
Genetic and Proteomic Insights into Cardiac Ageing
Genetic analyses demonstrate that the accumulation of somatic mutations increases steadily with age, compromising cardiomyocyte function. This genomic instability correlates with mitochondrial decline and metabolic inefficiency.
Proteomic studies reveal distinct stages in biological ageing, identifying proteins that change predictably across decades of life. These biomarkers enable estimation of biological age and may help evaluate therapeutic responses to senescence-targeting treatments. Monitoring molecular ageing signatures could become an essential component of cardiovascular risk assessment in the future.
Integration of Senescence in Cardiovascular Pathogenesis
Cellular senescence intersects multiple cardiovascular conditions. It contributes to endothelial dysfunction in hypertension, plaque formation in atherosclerosis, scarring in myocardial infarction, and contractile failure in heart failure. Across these diseases, the hallmarks remain consistent: DNA damage, oxidative stress, chronic inflammation, and impaired regeneration.
Senescent endothelial cells lose their capacity to regulate vascular tone, while senescent fibroblasts drive stiffening of cardiac tissue. Senescent smooth muscle cells alter vascular architecture, and aged cardiomyocytes exhibit reduced excitability and endurance. These changes collectively reshape cardiovascular physiology and elevate disease risk.
Challenges and Future Directions
Despite compelling evidence, translating senescence research into clinical cardiology faces major obstacles. Senescent cell markers are inconsistent across tissues, making detection difficult. The mechanisms underlying selective vulnerability of certain cell types remain unclear. Additionally, eliminating too many senescent cells could disrupt normal repair processes that rely on transient senescence.
Future studies must define precise therapeutic windows, refine delivery systems, and evaluate long-term outcomes. Combining molecular biology with computational modeling will accelerate progress toward safe, individualized treatments. Integration of gene editing, machine learning, and omics technologies can further enhance precision.
A deeper understanding of how metabolic and epigenetic factors influence senescence will help design multi-target therapies that promote cardiovascular rejuvenation without compromising safety.
Conclusion
Cellular senescence stands at the crossroads of ageing and cardiovascular pathology. Initially protective, it becomes destructive when unchecked. Its influence spans endothelial dysfunction, myocardial remodeling, and fibrotic progression. Advances in molecular biology now allow detailed mapping of senescence pathways and identification of actionable targets.
Eliminating or modulating senescent cells holds the promise of reversing aspects of cardiovascular ageing. Senolytics, senomorphics, metabolic regulators, and sirtuin activators collectively form a growing arsenal against age-related heart disease. Yet these strategies demand careful refinement to balance rejuvenation with biological stability.
The study of senescence reveals that ageing is not merely a passive decline but an active, regulated process open to intervention. By understanding and controlling cellular senescence, medicine may soon shift from managing cardiovascular decay to restoring youthful function. The heart, once thought destined to age irreversibly, could one day regain resilience through precision therapies that harness the biology of renewal.
The study is published in the journal Cell Death Discovery. It was led by researchers from Affiliated Hospital of Zunyi Medical University.