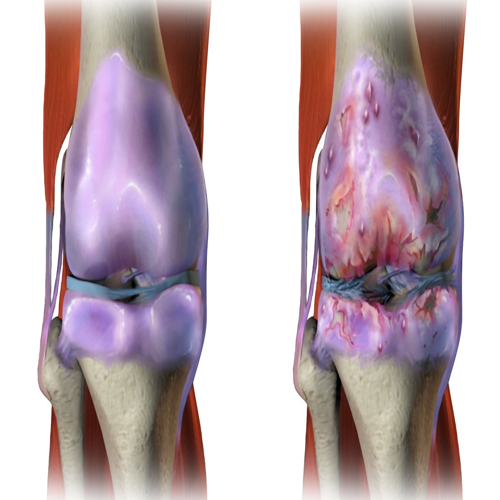
Osteoarthritis affects daily comfort for millions across the world. The condition gradually disrupts movement and reshapes how people live. Many notice early stiffness or mild discomfort during routine tasks. These signs often deepen over time. Joints lose strength and stability. Activities that once felt simple suddenly require care and patience.
Current treatments mainly reduce symptoms without correcting underlying damage. Doctors offer exercise routines, weight control plans, pain medicines, or lubricant injections. These options provide temporary comfort but rarely restore cartilage structure. Patients often wish for a therapy that actually slows joint decline. Many hope for something that protects tissue rather than simply easing discomfort.
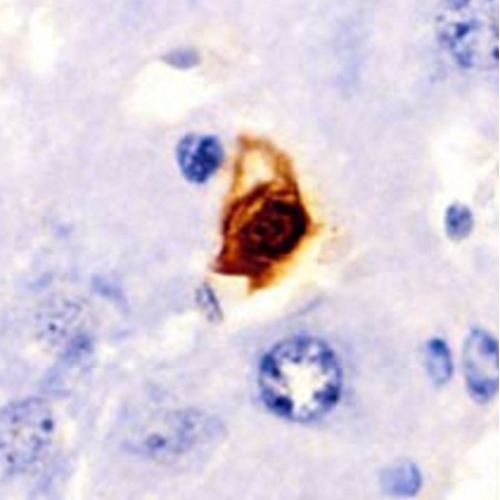
Researchers now investigate deeper biological forces within affected joints. They study cellular changes that occur long before major structural damage appears. Modern tools reveal complex patterns emerging inside cartilage layers. One pattern appears repeatedly across studies. Senescent cells accumulate inside cartilage as joints age or suffer injury. These cells disrupt the surrounding environment and guide tissue toward steady decline.
A new compound called SSK1 targets these harmful cells with selective precision. Researchers designed SSK1 to activate mainly within senescent cells. This property reduces harm to healthy cells and enhances safety. The new study explores the behaviour of SSK1 in laboratory experiments, human cartilage samples, and animal models. The results show strong potential for future therapies.
This article explains the science behind these findings. It describes the biology of senescence, the action of SSK1, the changes observed in human tissue, and the wider effects seen in living joints. The information suggests a future where osteoarthritis treatment may shift toward regeneration instead of damage control.
Why Senescent Cells Matter
Senescent cells arise when stress, injury, or excessive replication halts division. These cells stop multiplying but remain active inside tissue. They release inflammatory signals that disturb healthy neighbours. Researchers call this group of molecules the senescence associated secretory phenotype. It includes enzymes that break cartilage and cytokines that sustain inflammation.
The presence of these cells affects cartilage in several ways. They weaken the structural matrix that supports smooth movement. They reduce collagen production and increase collagen breakdown. They disrupt the balance between synthesis and degradation. Over time, the combined effects promote erosion and thinning.
Healthy cartilage usually contains very few senescent cells. The joint remains balanced because cell renewal and matrix turnover work in harmony. However, osteoarthritis shifts this balance sharply. Damaged cartilage shows increased numbers of senescent chondrocytes. These cells produce far more inflammatory molecules than healthy counterparts. Their activity accelerates structural decline.
These cells also influence surrounding tissues. Subchondral bone beneath the cartilage responds to altered signals by changing density and architecture. Synovial tissue around the joint receives inflammatory cues and increases irritation. Mechanical forces amplify these molecular disturbances.
Senescent cells remain stable once formed. They resist programmed cell death because their internal pathways change. This resistance makes them difficult to remove naturally. Their prolonged presence creates a self reinforcing cycle. Cartilage becomes more vulnerable to stress. Stress triggers more senescence. The loop continues.
Researchers recognised that removing these cells might disrupt this cycle. If senescent cells disappear, healthy cells may regain normal function. The surrounding tissue may become less inflammatory. The matrix may regain stability. This idea guides the development of modern senolytic strategies.
How SSK1 Works
SSK1 acts as a prodrug. This means the compound stays inactive until exposure to a specific trigger. Senescent cells produce high levels of beta galactosidase. This enzyme becomes the trigger. When SSK1 enters a senescent cell, the enzyme transforms it into its active form. This transformation releases a compound that reduces viability in those cells.
Healthy cells produce lower beta galactosidase levels. They rarely activate SSK1. This difference creates selectivity. The compound targets harmful cells while sparing normal ones. Selectivity remains vital for joint therapy because cartilage repair requires living chondrocytes.
Researchers tested SSK1 under various conditions. They induced senescence through oxidative stress, replication fatigue, or drug exposure. SSK1 reduced viability in senescent cells across all methods. The compound left healthy chondrocytes largely intact. This behaviour confirms the precision of the mechanism.
The compound also affects senescent cells in related tissues. Senescent mesenchymal stem cells respond similarly to treatment. Senescent fibroblasts also show reduced viability. These responses suggest broader therapeutic potential. Many joint tissues undergo stress during osteoarthritis. Clearing senescent cells from several sources may benefit overall joint health.
SSK1 also reduces signals associated with cellular damage. Senescent cells often display markers linked to DNA injury. These markers decrease after treatment. This pattern suggests reduced stress within remaining tissue. Lower stress may help surrounding healthy cells regain balance.
SSK1 produces additional effects on the internal environment. Senescent cells gradually alter pH levels, energy metabolism, and oxidative balance. Removing them may stabilise these factors. Subtle shifts in the microenvironment often influence long term tissue outcomes. Positive shifts support resilience against future degeneration.
The mechanism of SSK1 highlights a key advantage. It uses the biology of the harmful cell to drive its own removal. This approach prevents widespread toxicity and focuses action on the source of decline.
Effects In Human Tissue
Human cartilage experiments offer strong insight into therapeutic potential. Researchers obtained samples from patients with severe osteoarthritis. These samples contain many senescent chondrocytes and show typical signs of degeneration. Scientists cut the samples into small pieces and maintained them in controlled culture. They exposed some pieces to SSK1 and kept others untreated for comparison.
The treated cartilage pieces showed reduced senesescence over time. Many senescent markers declined steadily. These declines indicate removal of harmful cells. Fewer senescent cells improve the overall behaviour of the tissue.
Researchers observed reduced expression of inflammatory genes. Molecules like IL 6 and TNF alpha decreased. These cytokines play strong roles in osteoarthritis progression. Lower levels suggest a calmer environment with reduced stress signals. Enzymes that break cartilage, such as MMP13, also declined. These enzymes accelerate structural damage during disease progression.
At the same time, anabolic markers increased. Chondrocytes began producing more structural molecules. Collagen type II and aggrecan rose in expression. These molecules form the basic framework of healthy cartilage. Their presence marks increased repair capacity.
Proliferation markers also increased after SSK1 treatment. These changes indicate improved cell activity. Chondrocytes with renewed vitality contribute to thicker and stronger matrix formation. This pattern reverses one of the core problems in osteoarthritis. Diseased cartilage loses the ability to maintain its matrix. Restored proliferation helps counter this decline.
Proteoglycan content improved in treated tissue. Proteoglycans help retain water and support joint cushioning. Their increase suggests stronger mechanical resilience. Cartilage with higher proteoglycan content withstands compression more effectively.
The combined changes point toward a more balanced tissue state. The cartilage moves away from inflammatory breakdown and toward regeneration. This shift includes molecular, cellular, and structural improvements.
Such results in human tissue samples strengthen the case for broader exploration. Many compounds perform well only in animal models. Human tissue offers a stronger reflection of clinical reality. These findings position SSK1 as a strong candidate for future research.
Results In Animal Models
Animal models help researchers understand the behaviour of SSK1 in living joints. Scientists induced post traumatic osteoarthritis in young rats by cutting the anterior cruciate ligament. This injury triggers rapid cartilage loss and inflammation. After the injury, rats received regular injections of SSK1 directly into the joint.
The treated rats displayed slower progression of joint decline. Their cartilage maintained stronger structure. The matrix appeared thicker and more uniform. Degeneration markers decreased, and regenerative markers increased. Treated rats moved more comfortably and showed reduced pain responses. Pain sensitivity often increases during osteoarthritis because damaged tissue irritates local nerves. Reduced sensitivity suggests improvement in tissue health.
Subchondral bone also improved after treatment. Osteoarthritis often disrupts the bone beneath cartilage. The bone becomes uneven, dense in some areas, and weak in others. These changes worsen joint mechanics. Treatment reduced these irregularities. Bone structure appeared more consistent and stable.
Scientists repeated the experiments in aged mice. Age adds complexity to osteoarthritis progression. Older animals show slower healing, greater inflammation, and higher senescence levels. However, SSK1 improved cartilage structure even in aged joints. Treated mice displayed stronger matrix content, lower senescence, and reduced destructive enzymes. They also showed improved bone structure beneath the cartilage.
Inflammation decreased across treated animals. Synovial tissue appeared less thick and irritated. Lower inflammation supports smoother movement. It also reduces pain and protects cartilage from further damage.
Apoptotic markers also decreased after treatment. Senescent cells naturally resist apoptosis. Clearing them through SSK1 reduces the stress burden in the tissue. Lower apoptotic levels mean healthier surviving cells. The cartilage environment becomes more supportive of regeneration rather than decline.
The joint compartments showed better integration between cartilage and bone. This integration matters for load distribution during movement. Healthier interfaces reduce microdamage and improve stability.
Treated animals also avoided systemic toxicity. Major organs displayed normal appearance and normal blood values. This safety profile supports further exploration of the compound.
These results across young and old animals align with human tissue findings. SSK1 consistently improves joint health by removing harmful cells and supporting regenerative processes. The wide range of positive outcomes highlights its potential as a future therapy.
Promise Ahead
The study presents a compelling direction for osteoarthritis research. SSK1 works through a targeted mechanism that clears harmful senescent cells. This process restores balance within cartilage, bone, and synovial tissue. The compound acts with selectivity, safety, and strength.
Its effects span several layers of joint biology. It reduces inflammation, increases structural proteins, enhances proliferation, and stabilises the microscale environment. It improves bone behaviour and reduces pain signals. Each benefit contributes to a healthier joint.
The findings suggest a future where osteoarthritis treatment may shift dramatically. Rather than masking symptoms, therapy may focus on removing the cellular drivers of degeneration. By clearing senescent cells, researchers may restore natural repair pathways and extend joint lifespan.
Further research will explore dosing schedules, long term safety, and delivery methods. Larger models will help refine understanding. Human trials may eventually determine clinical potential.
The core idea remains powerful. Targeted removal of harmful cells can reshape disease progression. SSK1 illuminates this path with strong early evidence. It offers a step toward treatments that protect joints, preserve movement, and support long term mobility.
This work shows that regeneration is possible when harmful forces decline. Senescent cells once seemed unavoidable, but targeted removal reveals new possibilities. The coming years may transform osteoarthritis care with these insights.
The study is published in the journal EBioMedicine. It was led by researchers from Peking University.